Lobular carcinoma in situ (LCIS)
Find a cancer specialistLobular carcinoma in situ (LCIS) is a non-cancerous condition where abnormal cells grow in the milk glands of your breast. While LCIS is not breast cancer, your risk of getting cancer increases if you’re diagnosed with it.
If you’re diagnosed with LCIS, your Aurora cancer specialist may recommend more screenings and treatments to lower your risk of developing invasive breast cancer.
What is LCIS?
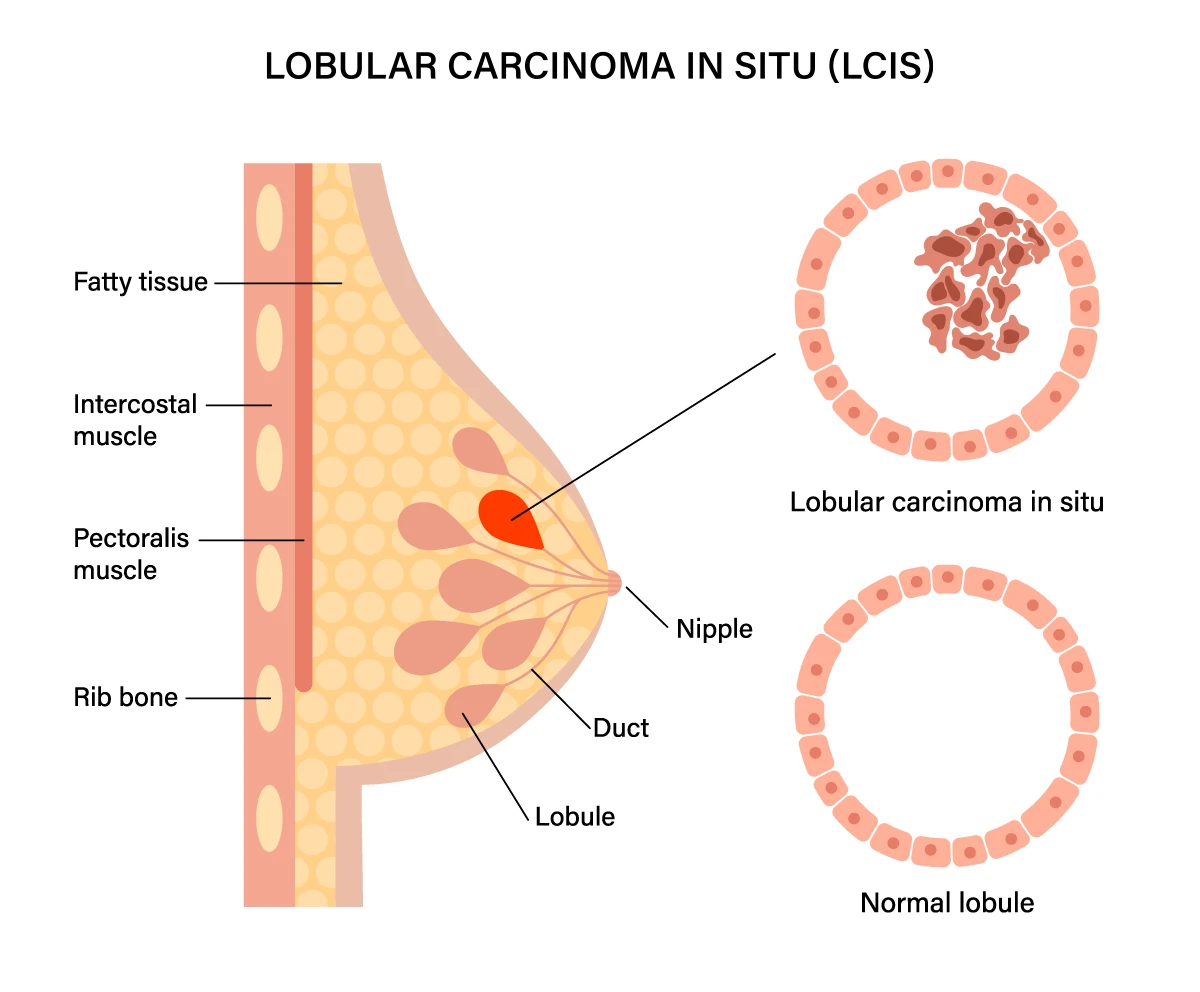
Lobular carcinoma in situ (LCIS) is a non-invasive cancer that grows inside the milk glands (lobules) in the breast and hasn’t spread to nearby tissue.
With LCIS, abnormal cells are found in the lobules of the breast. The term “in situ” means “in place," so the abnormal cells do not penetrate the walls of the lobules or invade the surrounding breast tissue.
LCIS is not considered cancer, but it does indicate a greater risk for developing breast cancer in the future. Yet, it doesn't always lead to cancer itself.
Mammograms usually don’t catch LCIS. It's usually discovered with a breast biopsy for a different reason, such as a lump in the breast or abnormal mammogram.
While breast cancer, including its precancerous conditions like LCIS, are much more common in women, it is still possible for men to develop LCIS and other types of breast cancer.
How long does LCIS take to become invasive?
There is no way to tell how long it will take for LCIS to become invasive breast cancer, if it does at all. Most cases of LCIS never progress into invasive breast cancer.
The risk of developing invasive breast cancer is higher if you have LCIS compared to those who don’t. However, the actual risk varies from person to person and depends on various factors such as age, family history, genetics, hormone fluctuations and lifestyle factors.
Regular monitoring and follow-up care are crucial if you have LCIS so any signs of progression or development of invasive cancer can be detected early. This typically involves regular breast exams, mammograms and sometimes additional imaging or biopsies.
What are the risk factors for LCIS?
Multiple factors contribute to the risk of developing LCIS, ranging from family history, genetic mutations and lifestyle factors. If you have a family history of breast cancer, genetic testing can help assess your risk, especially for gene mutations associated with increased risk of breast cancer.
Other risk factors for LCIS include:
- Age: LCIS is more common in women who are between 40-60 years old. While it can occur at any age, it's rare in younger women.
- Hormonal factors: Like many other breast conditions, LCIS is influenced by hormonal factors. Women with a higher lifetime exposure to estrogen, such as those who started menstruating early, had late menopause or never had children, may have an increased risk.
- Family history: A personal or family history of breast cancer, particularly in parents, siblings and children, can increase the risk of LCIS.
- Personal history of breast cancer: If you have previously been diagnosed with noncancerous breast conditions you have an increased risk of LCIS.
- Hormone replacement therapy (HRT): Long-term use of hormone replacement therapy after menopause may slightly increase the risk of LCIS.
- Breast density: Women with dense breast tissue, as seen on mammograms, may have a higher risk of getting LCIS.
LCIS symptoms
LCIS doesn’t cause symptoms since it’s restricted to the breast’s lobules. Your doctor may discover LCIS through an abnormal mammogram or biopsy for a lump in your breast.
Schedule an appointment with your doctor if you notice any changes in your breasts, such as a breast lump, nipple discharge or changes in appearance.
LCIS diagnosis
Diagnosing LCIS poses a challenge since it doesn't show any symptoms. When abnormalities are found on a mammogram, a LCIS diagnosis is confirmed through a core needle breast biopsy.
During a core needle breast biopsy, a small tissue sample is removed with a thin, hollow needle from the area where the abnormal cells were identified. A pathologist will look at the tissue to confirm a diagnosis of LCIS.
LCIS treatment
Your personalized treatment plan for LCIS will vary depending on factors such as your overall health, preferences and risk factors.
The following treatments are commonly used for LCIS:
- Observation: Your doctor will recommend more regular checkups and monthly self-exams. They may also suggest annual mammograms to check for any changes in the breast tissue.
- Preventive mastectomy: Includes the removal of one or both breasts to reduce the risk of developing invasive breast cancer. Skin-sparing and nipple-sparing mastectomies may be offered, depending on the proximity of the LCIS to those areas.
- Surgical treatments: A lumpectomy may be an option, where your surgeon removes any cancerous and abnormal tissue, some healthy tissue and lymph nodes under the arm. After surgery, your doctor will deliver radiation therapy into an open incision.
- Risk-reducing medications: Selective estrogen receptor modulators or aromatase inhibitors may be prescribed to block estrogen receptors in the breasts. This helps reduce your risk of developing invasive breast cancer.
Are you at risk for breast cancer?
Knowing your chance of developing breast cancer can help you plan a routine screening schedule. Our breast health quiz estimates your five-year and lifetime risk and gives you an idea of what to do next based on your results.
Get care
We help you live well. And we're here for you in person and online.