Esophageal varices
Find a GI specialistEsophageal varices can be a serious, sometimes life-threatening, result of advanced liver disease. At Aurora Health Care, our expert esophageal varices specialists tap into the latest diagnostic tools and treatments to provide advanced esophageal varices therapies for the best possible care.
Understanding esophageal varices
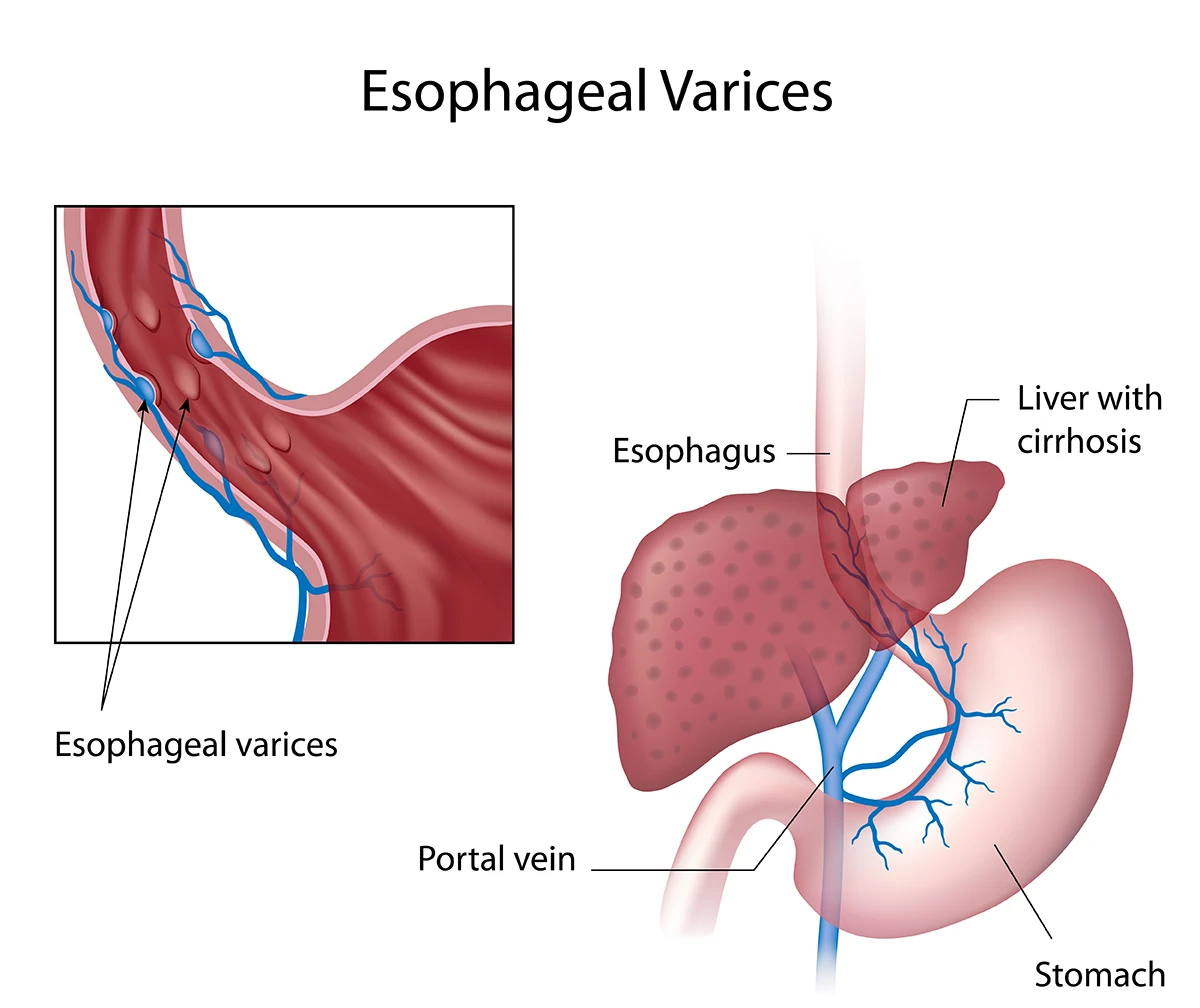
Esophageal varices are enlarged veins in the esophagus. When these veins become blocked, they restrict blood flow to the liver.
In the lower part of your esophagus there are veins that help transport blood from the pancreas to the liver, comparable to an interstate highway. When these highways – or veins – become swollen, this is known as esophageal varices.
These swollen vessels develop because of blockages in the blood routes going to the liver. Because of these blockages, blood finds other routes to the liver.
This situation causes pressure to build in smaller vessels, which can make these vessels burst. A burst could lead to dangerous bleeding and cause symptoms, such as vomiting blood or showing blood in your stool.
If you have these symptoms, call 911 immediately.
Causes of esophageal varices
Blood clots, liver disease and certain infections can lead to esophageal varices. Other problems such as heart disease and Type II diabetes can also block the blood paths in the esophagus.
Primary esophageal varices causes
- Liver scars and diseases: The top culprit of esophageal varices is liver scarring from diseases such as hepatitis C, which causes the liver to work harder and possibly shut down.
- Blood pressure spikes: Another usual cause is a rise in blood pressure in veins that run from the pancreas to the liver. This is known as portal hypertension and is often related to liver problems.
Secondary esophageal varices causes
- Blood clots: A block in the main blood route can force blood into other paths, such as those in the esophagus.
- Less common causes: Some infections, certain cardiovascular conditions and growths might also play a role in the development of esophageal varices.
Esophageal varices risk factors
Having esophageal varices doesn't always mean you'll experience bleeding. However, certain things increase the risk. These include:
- Excessive alcohol intake
- Diets rich in fatty and fried foods
- Sedentary lifestyle
- Chronic hepatitis B or hepatitis C infections
- Nonalcoholic fatty liver disease
- Genetic predispositions
- Contributing conditions, such as schistosomiasis or Budd-Chiari syndrome, which can increase the risk of bleeding
Esophageal varices symptoms
Typically, esophageal varices symptoms are unnoticeable until the varices rupture. Signs you may have ruptured esophageal varices include:
- Throwing up blood
- Dark, sticky stool
- Signs of low blood (light headedness, dizziness and passing out)
- Feeling extremely tired
- Your skin turns yellow, especially under the eyes (jaundice)
- Belly bloating
- Feeling confused or slurring words
If you experience any of these symptoms, schedule an appointment with an Aurora specialist. If you see blood in your vomit or stool, call 911 and seek emergency care immediately.
Esophageal varices diagnosis and treatment options
If your liver is in bad shape, your doctor likely checks for esophageal varices from time to time. If symptoms develop, your doctor will perform a physical exam, review your medical history and may run tests to check for esophageal varices.
Diagnosis tools such as a capsule endoscopy, CT scan and ultrasound can be used to check for the development or severity of esophageal varices.
Esophageal varices treatment
Our team uses innovative esophageal varices treatments. Your doctor may suggest lifestyle changes for better esophageal varices management or even recommend surgery to clear blockages.
One treatment for esophageal varices is prescription beta blockers to lower blood pressure and reduce bleeding risks. Your doctor might also recommend esophageal varices banding, which involved placing a band around the swollen vessels to stop or prevent bleeding.
If bleeding risks increase, your doctor might recommend surgery or even a liver transplant for advanced liver disease. The most common surgical procedure is the placement of transjugular intrahepatic portosystemic shunts (TIPS), which creates a shortcut to ease blood flow into the liver and lowers blood pressure.
Esophageal varices prevention
The best way to prevent esophageal varices from developing or rupturing is to keep your liver healthy:
- Don’t drink alcohol: It's extra work for your liver.
- Eat right: Go for lean meats, fruits and vegetables, and cut out fatty foods.
- Reduce exposure to chemicals: Your liver cleans out toxins. Wear gloves with cleaning products and when working around chemicals.
- Stay fit: Extra weight strains your liver and increases your risk of liver disease.
- Be safe: Avoid hepatitis B and hepatitis C by not sharing needles and practicing safe sex
Other prevention methods focus on preventing bleeding with the use of medications and esophageal varices banding.
Get care
We help you live well. And we’re here for you in person and online.