Hip osteoarthritis
Find an ortho specialistHip osteoarthritis is a prevalent and often painful chronic condition that significantly affects your daily life. With the right treatment plan, you can manage your symptoms and maintain a good quality of life.
Our team of orthopedic specialists at Aurora Health Care is here to help you have a speedy recovery. We offer the latest treatment and diagnostic methods, providing you with many options to meet your needs.
Schedule an appointment
From recent injuries to nagging aches and pains, our orthopedic specialists can help. Schedule your orthopedic appointment in LiveWell, online or by phone.
What is hip osteoarthritis?
Osteoarthritis is a long-term condition that affects the joints in your body and worsens over several years. It’s the most common form of arthritis, especially affecting older adults.
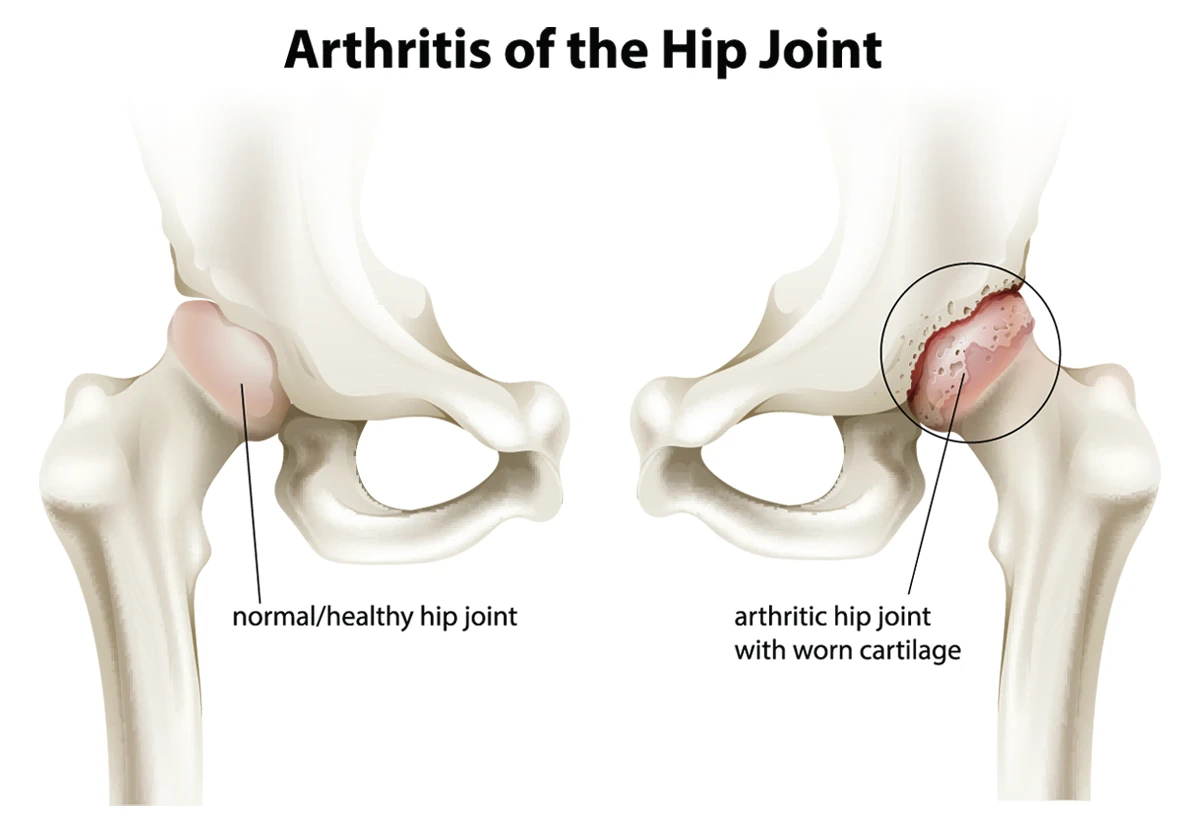
Hip osteoarthritis happens when the cartilage in your hip joint gradually deteriorates over time. It’s sometimes referred to as degenerative joint disease.
Your hips are one of two sets of ball and socket joints in your body. The other set is at your shoulders. Cartilage surrounds the joints where they connect and works like a cushion to keep the bones from rubbing against each other.
As you get older, the cartilage wears down and the bones start to rub against each other, causing pain, stiffness and reduced mobility in your hip.
Causes of hip osteoarthritis
The exact cause of hip osteoarthritis isn't entirely known, but several factors can contribute to its development, including:
- Age: The likelihood of developing osteoarthritis increases as you get older due to the cumulative wear and tear on your hip joints.
- Developmental disorders: Conditions like hip dysplasia, where the hip joint doesn't form correctly, can increase the risk of osteoarthritis of the hip.
- Genetics: If your family members, such as parents or siblings, have had osteoarthritis of the hip, you may have a higher risk because of hereditary factors.
- Joint injuries: Past injuries to your hip, such as fractures or dislocations, can lead to osteoarthritis later in life.
- Loss of muscle mass: Muscles help protect the joints in your body. A decrease in muscle mass can weaken the joint and lead to osteoarthritis of the hip. You naturally start losing muscle mass in your late 30s.
- Obesity: Extra weight places additional stress on your hip joints, accelerating cartilage breakdown.
- Repetitive stress: Jobs or activities involving repetitive movements or heavy lifting can strain your hips, contributing to osteoarthritis.
What age do people get osteoarthritis in their hips?
Hip osteoarthritis can develop at any age, but it is most commonly found in people over 50. The risk increases with age due to the cumulative effect of joint wear and tear. However, younger individuals can also develop osteoarthritis of the hip, especially if they have risk factors like joint injuries, genetic predisposition or developmental hip disorders.
In your 30s and 40s, you might notice early signs of hip osteoarthritis, particularly if you engage in high-impact activities or have had significant hip injuries. For most people, hip osteoarthritis symptoms become more pronounced and debilitating in their 50s and beyond.
Hip osteoarthritis symptoms
Recognizing the symptoms of hip osteoarthritis is key to seeking early treatment and managing the condition effectively. Common symptoms include:
- Grinding or clicking: You might hear or feel a grinding sensation in your hip joint during movement.
- Limited range of motion: You may notice a reduced ability to move your hip in certain directions, affecting daily activities like walking, sitting or putting on shoes.
- Pain: You might feel deep, aching pain in your groin, buttocks or inner thigh. The pain can be constant or intermittent, often worsening with activity.
- Stiffness: Your hip may feel stiff, especially after periods of inactivity or in the morning. This can make moving or bending your hip difficult.
- Weakness: The muscles around your hip may weaken over time, further limiting your mobility and increasing pain.
These symptoms can vary in intensity and may come and go initially, often becoming more persistent and severe as the condition progresses. If you notice any of the above symptoms, schedule an appointment with your doctor.
Diagnosing hip osteoarthritis
Diagnosing hip osteoarthritis typically involves a combination of your medical history, physical examination and imaging tests.
Your doctor will ask about your symptoms, including when they started, their severity and how they affect your daily life. They’ll also inquire about any previous hip injuries, your family history of arthritis and any other medical conditions you might have.
During the exam, your doctor will assess your hip’s range of motion, check for tenderness or swelling and observe how you walk. They may also test your muscle strength and joint stability.
X-rays are commonly used to confirm a diagnosis of hip osteoarthritis. They can reveal joint space narrowing, bone spurs and other changes indicative of osteoarthritis. In some cases, an MRI might be ordered to provide a more detailed view of the cartilage and other soft tissues in your hip.
Hip osteoarthritis treatments and therapies
Hip osteoarthritis treatment involves a combination of lifestyle changes, medications and sometimes surgical interventions.
- Healthy weight: Maintaining a healthy weight can reduce stress on your hip joints.
- Exercise: Regular low-impact exercises, such as swimming or cycling, can improve joint mobility and strengthen the muscles around your hip. Physical therapy can also teach you exercises and techniques to manage symptoms.
- Medications: Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. In some cases, your doctor might prescribe stronger medications or corticosteroid injections for more severe pain.
- Mobility aids: Using a cane or walker can help take the load off your hip and improve mobility. Shoe inserts or orthotics can also help by providing better support and alignment.
- Surgery: If conservative treatments fail to relieve your symptoms, surgical options like hip resurfacing or total hip replacement may be considered. These procedures can significantly reduce pain and improve your quality of life.
Is that pain cause for concern
Back, neck, hip or knee pain can cause severe discomfort and affect the way you live your life. Our pain quizzes evaluate your symptoms and risk factors and give you an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.