Osteoarthritis symptoms & treatment
Find an ortho specialistIf you've ever experienced regular unexplained joint pain or stiffness, you might have wondered what's going on inside your body. This is a common sign of osteoarthritis (OA), a common type of arthritis that can affect any of the joints in your body.
Osteoarthritis affects the joints of millions of people. While osteoarthritis can damage any joint, it’s commonly found in your hands, hips, knees and spine.
While there is no cure, and the damage to the joints can’t be reversed, symptoms of osteoarthritis can be managed with lifestyle changes and treatments to slow the disease’s progression, manage joint pain and improve joint function.
Schedule an orthopedic appointment
From recent injuries to nagging aches and pains, our orthopedic specialists can help. Schedule an appointment in LiveWell, online or by phone.
What is osteoarthritis?
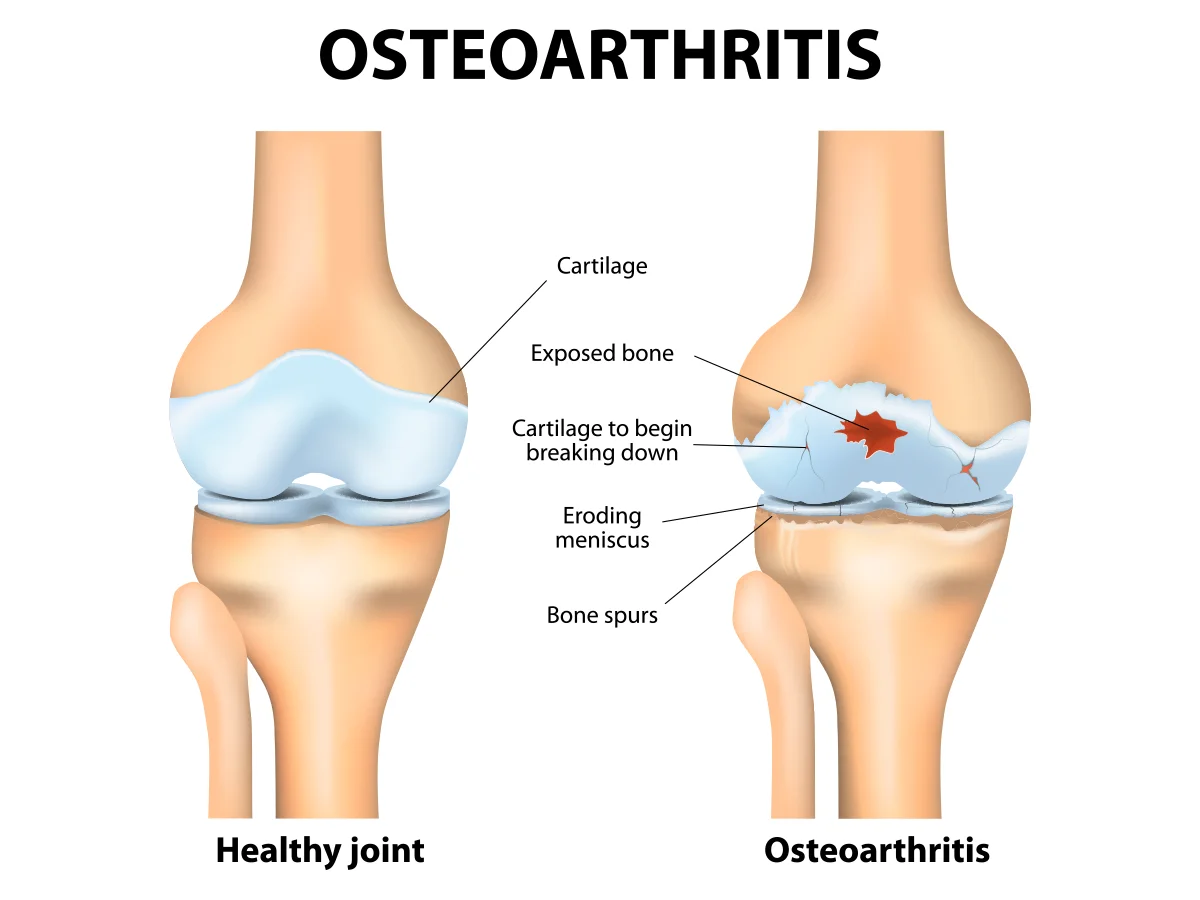
Osteoarthritis, also known as degenerative joint disease, happens when the cartilage in your joint breaks down and causes the connecting bones to rub against each other, causing pain and inflammation.
Imagine your joints like the hinges on a door – they're what allow your bones to move smoothly and without pain. But when you have osteoarthritis, those hinges start to wear down, causing pain, stiffness and sometimes swelling in the affected joints.
Cartilage is the cushiony layer between your bones and works like a shock absorber. In a healthy joint, this cushiony layer helps your bones glide smoothly against each other.
Osteoarthritis doesn't happen overnight. This condition develops over many years due to overuse, injuries, genetics and other risk factors. There are plenty of ways to manage osteoarthritis and keep those joints moving smoothly.
Osteoarthritis risk factors
Your risk of developing osteoarthritis increases due to factors such as:
- Age: As you get older, the risk of developing osteoarthritis gets higher.
- Gender: Women have a higher risk of getting osteoarthritis than men.
- Obesity: Excess body weight puts more pressure on weight-bearing joints such as your hips and knees.
- Injuries: Sports injuries or accidents that affect any of your joints can increase the risk of osteoarthritis regardless of when they occur.
- Repeated stress: Some jobs and sports require repetitive stress on a joint. Over time, this stress can lead to osteoarthritis.
- Genetics: Osteoarthritis tends to run in families.
- Bone or joint deformities: Some people are born with malformed joints or defective cartilage.
- Metabolic disease: Diabetes and hemochromatosis (too much iron) can increase your risk of osteoarthritis.
What are 5 symptoms of osteoarthritis?
The five most common osteoarthritis symptoms include:
- Joint pain: This is one of the most noticeable signs of osteoarthritis, especially when moving. The pain can range from mild discomfort to sharp, stabbing sensations.
- Joint stiffness: Stiffness, especially after periods of inactivity like sitting or sleeping, is a classic symptom of osteoarthritis.
- Swelling: Inflamed joints are a common sign of osteoarthritis and can make movement even more uncomfortable.
- Decreased range of motion: You might notice that you can't move your knees, hips or other affected joints as freely as you used to.
- Cracking sound in your joints: Hearing a crackly or crunching sound when moving your joints is another telltale sign of osteoarthritis. It’s often due to roughened cartilage rubbing against bone.
Osteoarthritis is typically a slow-progressing condition, and symptoms may worsen over time. The rate at which the condition progresses can vary widely from person to person.
In some individuals, the progression may be relatively slow, with symptoms gradually worsening over many years. For others, the progression may be more rapid, especially if there are factors such as significant joint damage, obesity or certain genetic factors at play.
If you're experiencing any of these symptoms, schedule an appointment with an Aurora Health Care orthopedics specialist.
Diagnosing osteoarthritis
Your provider will perform a medical exam and review your osteoarthritis symptoms and medical history to diagnose this condition. As part of the physical exam, your provider will observe how your joints move, your range of motion and stability, and check your reflexes.
After your physical exam, your provider may use digital imaging tests to collect more information about how the joint is working. These tests include:
- X-Rays: This is a picture of your bones to see if they are rubbing together or if they’ve grown bone spurs.
- CT scans: This test combines X-rays from different angles into images of soft tissue and bone.
- An MRI: This scan can take detailed images of the bones and soft tissue, including cartilage that might be damaged by arthritis.
Your doctor may also perform a blood test to determine if your arthritis is rheumatoid arthritis or your joint health is being affected by another condition.
Osteoarthritis treatment
Treatment for osteoarthritis focuses on managing pain and slowing the progression of the disease. Damage to the joints cannot be reversed and there is no cure. Common osteoarthritis treatments include:
- Osteoarthritis medications: Pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce inflammation and alleviate pain. In some cases, your provider may prescribe stronger pain medications or topical treatments like creams or patches.
- Physical therapy: Working with a physical therapist can improve mobility and help relieve symptoms. They can design a personalized exercise program to strengthen the muscles around your affected joints, improve flexibility and reduce pain.
- Weight management: Carrying around extra weight puts added stress on your joints, so shedding a few pounds can make a significant difference. Your doctor or a nutritionist can help you come up with a plan for healthy eating and exercise to reach and keep a healthy weight.
- Assistive devices: Braces, splints or orthotic shoe inserts can help stabilize your joints and reduce pain during daily activities. If getting around is a struggle, a cane or walker can provide added stability and support.
- Injections: For more severe pain, your doctor might recommend injections directly into the affected joint. Corticosteroids can help reduce inflammation and relieve pain, while hyaluronic acid injections can provide lubrication and cushioning for the joint.
- Joint replacement surgery: In cases where other treatments haven't provided relief, joint replacement surgery might be an option. This surgery can help repair or replace damaged joint tissue and improve mobility and function.
- Alternative therapies: Some people find relief from osteoarthritis through alternative treatments like acupuncture, massage therapy or dietary supplements such as glucosamine and chondroitin.
What works for one person might not work for another, so it's essential to work closely with your care team to find the right osteoarthritis treatments for you.
Get care
We help you live well. And we’re here for you in person and online.