Osteoporosis symptoms & treatment
Request an appointmentYour bones are made up of living, growing tissue. As old bone tissue dies, your body constantly makes new, strong bone tissue. With osteoporosis, old bone is not replaced by new bone fast enough, causing a decrease in bone mass and bone density.
Over time, your bones become weaker and thinner and may fracture easily – even from bending, coughing, lifting light objects or a minor fall. Osteoporosis is called a silent disease because most people who have it don’t notice osteoporosis symptoms.
Osteoporosis symptoms
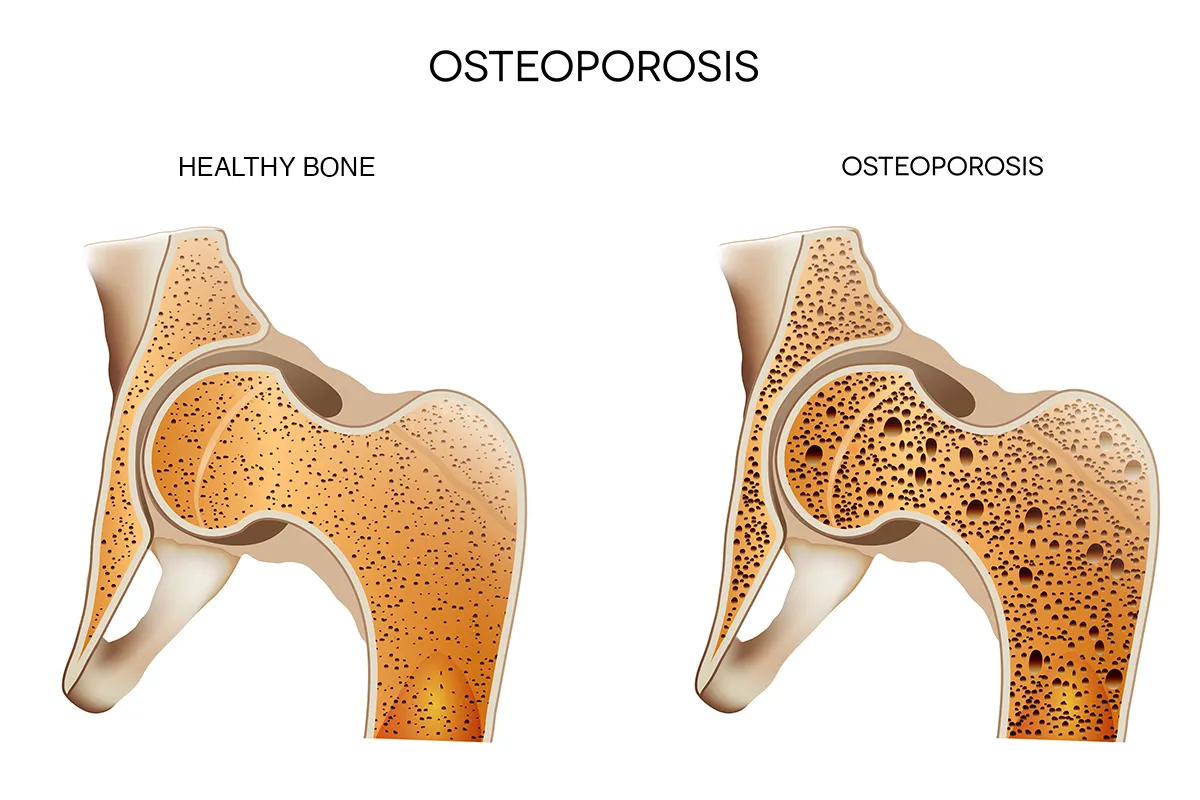
Osteoporosis makes bones gradually become less dense and more fragile. People with osteoporosis have a higher risk of broken bones, especially hips, wrists and vertebrae.
Symptoms of osteoporosis may include:
- A stooped or curved posture (kyphosis) when sitting or standing
- Height loss over time
- Collapsed or fractured vertebrae
- Bones that fracture easily
- Back pain
You may not notice any osteoporosis symptoms until you already have significant bone loss.
The four stages of osteoporosis
Osteoporosis develops gradually, and it’s often not diagnosed until you break a bone.
Stage 1: From about ages 20-40, bones break down at the same rate new tissue forms. This is considered the first stage of osteoporosis because bone growth is no longer faster than bone loss like it is from birth through adolescence. There are no symptoms at this stage.
Stage 2: At this stage bone loss begins to outpace bone growth. If you have an injury or get bone density testing done for another reason, you might be diagnosed with osteopenia, or slight bone loss.
Stage 3: If you reach this stage, you officially have osteoporosis. You still might not notice any osteoporosis symptoms, but you’ll be at increased risk for breaks and fractures – even from simple injuries like hitting your leg against a door. Symptoms at this stage may include having brittle nails, weakness in your hands, receding gums or tooth loss.
Stage 4: This is the most severe form of osteoporosis. Softer and weaker bones may show in the form of spinal deformities such as a bent-over appearance called kyphosis and pain with everyday activities. At this stage most people have had one or more broken bones because of osteoporosis.
What are the main causes of osteoporosis?
The main causes of osteoporosis are loss of bone mass and bone density. Your bones become thinner and weaker. The wrists, hips and vertebrae in the spine are the bones most affected by osteoporosis.
Your chances of getting osteoporosis may be increased by several risk factors, such as:
- Gender: Women are at greater risk for osteoporosis because they usually have thinner, less dense bones than men. Men are also at risk but don't usually get osteoporosis until after age 70.
- Age: Bone growth slows as you get older.
- Race: Osteoporosis is most common in non-Hispanic White people and in Asian women.
- Family history: If a parent has a history of hip fracture or osteoporosis.
- Hormones: Low levels of testosterone in men and low levels of estrogen in women.
- Diet: Excessive dieting for weight loss or consuming a diet low in calcium, protein or vitamin D.
- Certain types of medical conditions: Endocrine and hormonal diseases, gastrointestinal diseases, rheumatoid arthritis, cancer, HIV/AIDS and anorexia nervosa.
- Physical activity: Lack of exercise, or sedentary lifestyle.
- Alcohol abuse: Chronic frequent drinking.
- Smoking cigarettes: Smoking is linked to increased risk of osteoporosis.
Osteoporosis diagnosis
Doctors usually diagnose osteoporosis during a routine screening for the disease. Women may start screening at age 65 or sooner if they have a high risk of osteoporosis. When you visit your doctor, remember to report:
- Any previous fractures
- Your regular habits of diet, exercise and alcohol use
- Your smoking history
- Current or past medical conditions and medications
- Your family history of osteoporosis and bone fractures
- For women, your menstrual history
Your doctor may do a physical osteoporosis exam to check for:
- Loss of height and weight
- Changes in posture
- Balance and gait (the way you walk)
Osteoporosis testing may include:
- Blood work
- Dual-energy X-ray absorptiometry (DEXA) to measure bone mass and thickness
- X-ray, MRI or CT scan to show any new or existing fractures
Osteoporosis treatment
The goals for treating osteoporosis are to slow or stop bone loss and prevent bone fractures. Treatments range from changes to your daily habits to minimize bone loss in early stages of osteoporosis, to spinal surgery to treat pain and repair bone damage in advanced stages.
Self-care for osteoporosis
There are some things you can do yourself to protect your bone health, including:
- Doing weight-bearing exercises such as walking and lifting weights to increase strength, muscle mass, coordination and balance
- Limiting use of alcohol
- Not smoking
- Eating a nutritious diet rich in calcium, vitamin D and protein
Nonsurgical treatment for osteoporosis
When possible, your doctor will start with nonsurgical osteoporosis treatments such as:
- Fall prevention education to help avoid fractures
- Calcium and vitamin D supplements
- Medications, if prescribed, for pain or to treat osteoporosis
- Physical therapy
- Weight loss counseling
Surgical treatment for osteoporosis
More serious osteoporosis symptoms may require osteoporosis treatments like the following:
- Spinal fusion surgery: Two vertebrae are permanently connected to reduce pain, increase the stability of the spine and stop the formation of bone spurs.
- Spinal nerve block: Your doctor injects an anesthetic drug near or directly into your spinal nerve. Spinal nerve blocks may be used for pain relief or as a diagnostic tool to find what’s causing your pain.
- Spinal stabilization: Your doctor implants rods, screws or locking plates in the bones of your spine. An orthotic vest or brace may be used for less severe fractures.
- Vertebroplasty: Your doctor injects a medical-grade substance called bone cement, which holds the spine bones in their proper position to reduce pain and bone deformity.
- Kyphoplasty: First a balloon is inserted into the affected area to decompress your spine and allow you to regain lost height. Then your doctor will inject bone cement to stabilize your vertebrae.
Osteoporosis complications
In advanced stages, osteoporosis can cause other health conditions or occur along with conditions including:
- Cervical spinal stenosis and myelopathy (cervical spondylotic myelopathy): A narrowing of the spinal canal in the neck area, which may cause your spinal cord to become compressed or damaged. Symptoms may include pain, tingling, balance problems, numbness, muscle weakness and dizziness.
- Spinal compression fracture: A break or rupture in the bones of the spine (also called collapsed vertebrae). The most common sign is severe back pain.
- Hypocalcemic tetany: When extremely low blood levels of calcium cause involuntary muscle contractions.
- Radiculopathy: Pressure on a nerve root that causes pain, numbness or weakness. May also cause difficulty controlling specific muscles.
Find spine care near you
When you have osteoporosis, we’re here to make it easier for you to get back to the things that matter most. With your own care coordinator, you’ll be connected to an integrated team of specialists all working together on your personalized osteoporosis treatment plan. Learn more about our spine services locations.
Aurora St. Luke’s Medical Center
Aurora Medical Center – Summit
Is your back and neck pain cause for concern?
Back and neck pain can interrupt even the simplest things in life and can point to a serious problem. Our back and neck pain quiz evaluates your spine function, pain symptoms and risk factors and gives you an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.