Uterine cancer symptoms & treatment
Find a cancer specialistThere are two types of uterine cancer: endometrial cancer and uterine sarcoma. Endometrial cancer is more common than uterine sarcoma, which is a rare type of uterine cancer.
Our gynecologic oncology experts want to find uterine cancer before it spreads outside the uterus and while it's highly treatable. If you need surgery, we offer minimally invasive procedures for faster, easier recovery from uterine cancer.
Uterine cancer symptoms
Unusual bleeding patterns are usually the first signs of uterine cancer. These include:
- Bleeding not related to a menstrual cycle
- Bleeding after menopause
However, some symptoms related to uterine cancer may be related to other conditions, such as uterine fibroids. If you have unusual bleeding or any of the following potential uterine cancer symptoms, visit your Aurora Health Care OB-GYN or family practice doctor to be sure:
- Abnormal vaginal discharge
- Lump or mass in the lower abdomen
- Unexplained weight loss
- Trouble with urination
What does uterine cancer feel like?
Uterine cancer symptoms may feel painful or be a feeling of fullness such as:
- Pain, pressure or a feeling of fullness in the lower belly
- Pain during intercourse
- Pain during urination
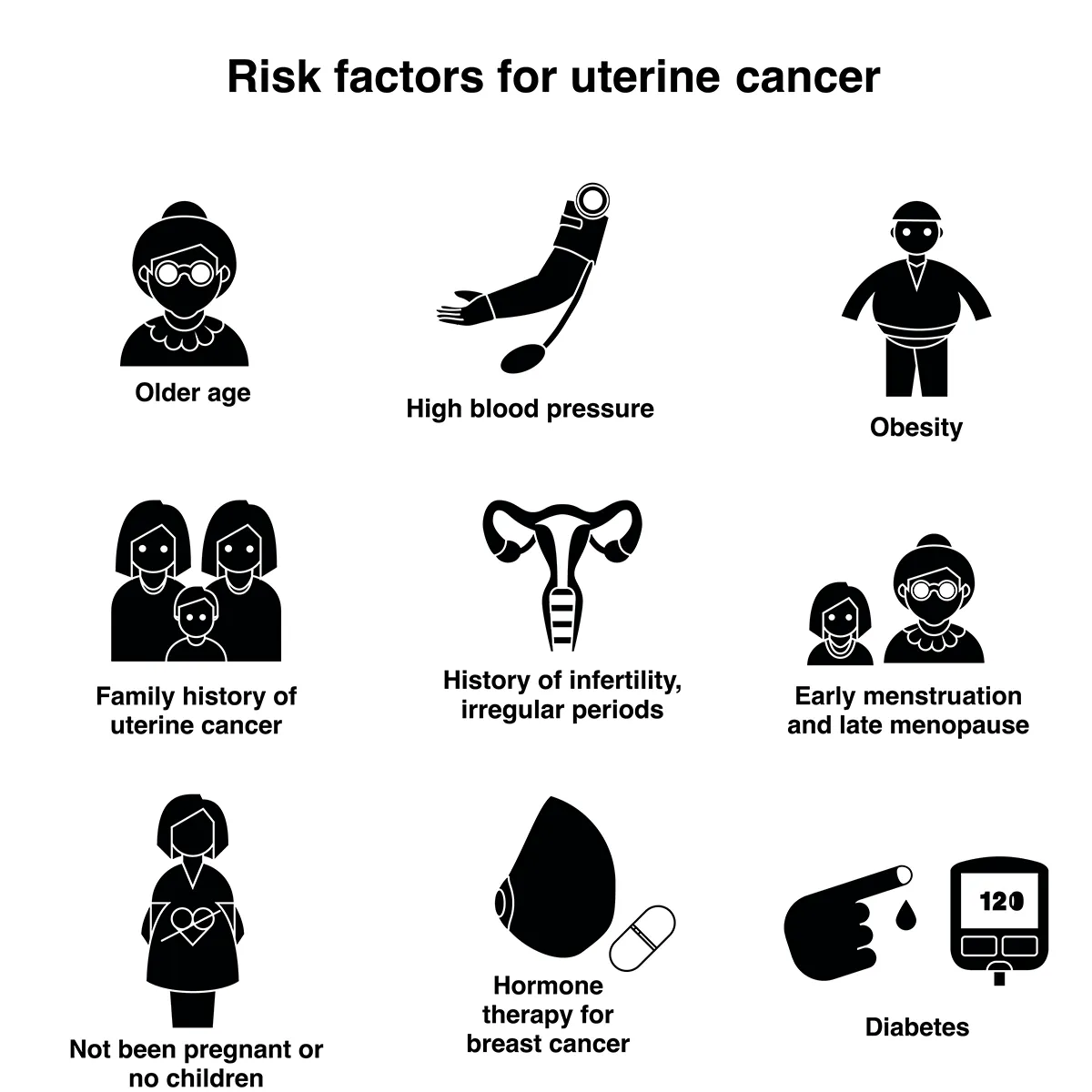
Uterine cancer risk factors
You may be more likely to get uterine cancer if you’ve previously had breast cancer. Having a family history of breast cancer, ovarian cancer or colon cancer also increases your risk. White women also have a higher risk of developing uterine cancers than women of other races.
Other risk factors include:
- Abnormal ovulation and menstruation patterns
- Age older than 50
- Diabetes or obesity
- Early age of first menstrual period or late onset of menopause
- Taking estrogen replacement therapy without progesterone
- History of endometrial hyperplasia
- Having polycystic ovarian syndrome (PCOS)
- Taking the drug tamoxifen (often used to prevent and treat breast cancer)
Find out if your doctor can test you for the BRCA1 or BRCA2 gene, which can also put you at risk for uterine, ovarian and breast cancer. Most cases of uterine cancer are highly curable if found early.
How we diagnose uterine cancer
When you talk with your OB-GYN about the symptoms you're having, they may ask about your personal and family medical history. They’ll also want to know about any abnormal vaginal bleeding outside of your normal cycle or if you’re in menopause. This information can help determine if you have any risk factors for uterine cancer.
Next, they'll perform a gynecological exam to rule out other causes of your symptoms. Your OB-GYN may want you to undergo certain tests, or they may refer you to a gynecologic cancer specialist for testing.
Tests to diagnose uterine cancer
- Endometrial biopsy uses a flexible tube inserted into the uterus through the cervix to collect a tiny portion of tissue from the lining of the uterus. The cells are examined under a microscope. If you have risk factors for uterine cancer, your doctor may recommend a yearly endometrial biopsy.
- Transvaginal ultrasound uses an ultrasound probe inserted into the vagina. The probe produces sound waves that create an image of the uterus to check for a tumor.
- Dilation and curettage (D&C) uses an instrument to remove cells from inside the uterus for further testing.
- Hysteroscopy uses a small scope inserted into the uterus through the cervix, which helps the doctor see anything abnormal, like a growth.
- CA-125 test is a blood test that looks for higher levels of a substance that could indicate the presence of cancer.
Tests to determine if uterine cancer has spread
- Cystoscopy or proctoscopy checks to see if cancer has spread to the urethra, bladder or rectum.
- CT scan not only confirms the presence of a tumor, but also can show its location and size and whether it has spread to nearby tissue.
- MRI produces images that help doctors determine whether a tumor is cancerous or noncancerous.
- PET scan uses a specific dye injected into a vein. The scan can identify cancer cells because they absorb the dye.
- Chest X-ray can show whether uterine cancer has spread to the lungs.
Uterine cancer treatments & services
Your treatment plan will depend on the diagnosis and your general health, as well as whether you have or want to have children. Your doctor will discuss the course of treatment that best suits your needs.
We may recommend surgery and then chemotherapy, radiation therapy or a combination of both to destroy additional uterine cancer cells. In some cases, we may use chemotherapy or radiation to shrink your tumor before surgery. In some cases, hyperthermic intraperitoneal chemotherapy (HIPEC) treatment can be used to combine chemotherapy and surgery.
Hormone therapy slows the growth of endometrial cancer cells by reducing hormones in the body. We may use it alone or with surgery and other therapies.
Surgical options for uterine cancer
A hysterectomy involves removing one or more of your female organs. Different hysterectomy types include:
- Single incision hysterectomy
- Simple hysterectomy to remove the uterus and cervix
- Total hysterectomy to remove the uterus, cervix, fallopian tubes and ovaries
- Radical hysterectomy to remove the uterus, cervix, fallopian tubes, ovaries and tissue around the uterus and cervix
Laparoscopy is a minimally invasive surgical procedure to remove some cancers or sample lymph nodes to see if cancer has spread. Through a few tiny incisions in the abdomen, the surgeon inserts a viewing scope, camera and special surgical instruments.
The tiny incisions often mean less pain and faster recovery. If necessary, the surgeon may still remove the uterus through a small incision at the top of the vagina.
Robotic surgery is another type of minimally invasive gynecological surgery similar to laparoscopy. It uses robotic precision combined with magnified views and the surgeon's skills to perform a hysterectomy.
Find out more about laparoscopy & robotic surgery.
Your surgeon will remove some of the lymph nodes in your pelvis and abdomen for examination under a microscope to see if the endometrial cancer has spread.
Hyperthermic intraperitoneal chemotherapy (HIPEC) is an innovative combination of surgery and chemo. The surgery starts by removing all visible tumors. Then a heated chemotherapy solution is placed in the open cavity to treat any remaining cancer cells. Then the chemo medication is drained and the incision is closed.
Nonsurgical treatments for uterine cancer
A special machine that sends beams of high-energy X-rays to target and destroy cancer cells. Your cancer specialist may recommend radiation therapy by itself or with surgery.
This type of radiation therapy uses small amounts of radioactive material inserted into or around the cancer, typically through your vagina. It's more targeted, so it affects less healthy tissue than external beam radiation.
These anti-cancer drug can be taken in pill form or via injections through a vein or injections under the skin. Chemotherapy drugs travel through your whole body to help control the spread of cancer to other organs.
These injections or pills help prevent or slow cancer growth by blocking hormones.
What to expect after treatment for uterine cancer
Endometrial cancer treatment may prevent you from getting pregnant later. If your fertility is important to you, talk to your doctor before being treated for uterine cancer. They’ll recommend a fertility evaluation and tell you about options that may help preserve your fertility.
Removing your ovaries will cause the immediate onset of menopause. Your doctor can help address any concerns you may have, along with how to find relief from menopausal symptoms.
Support and guidance
Across Aurora, you’ll find a full range of free or low-cost cancer support and social services to help you as you recover:
- Art therapy
- Dietary counseling
- Spiritual care
- Support groups
Get care
We help you live well. And we're here for you in person and online.