Psoriasis treatment
Find a dermatologistPsoriasis is a chronic skin condition that causes areas of your skin to become discolored, swollen and raised. It usually isn’t painful, but it may feel uncomfortable.
Though psoriasis commonly appears on the scalp, face and knees, it can also occur in other areas of your body such as your nails. Psoriasis often appears in childhood – small bumps on the skin are an early sign of psoriasis. As the condition worsens, your skin may develop an appearance of silvery scales, known as plaque.
Psoriasis isn’t contagious. The condition has no cure, but with proper treatment with a dermatologist, it can be controlled.
What is psoriasis?
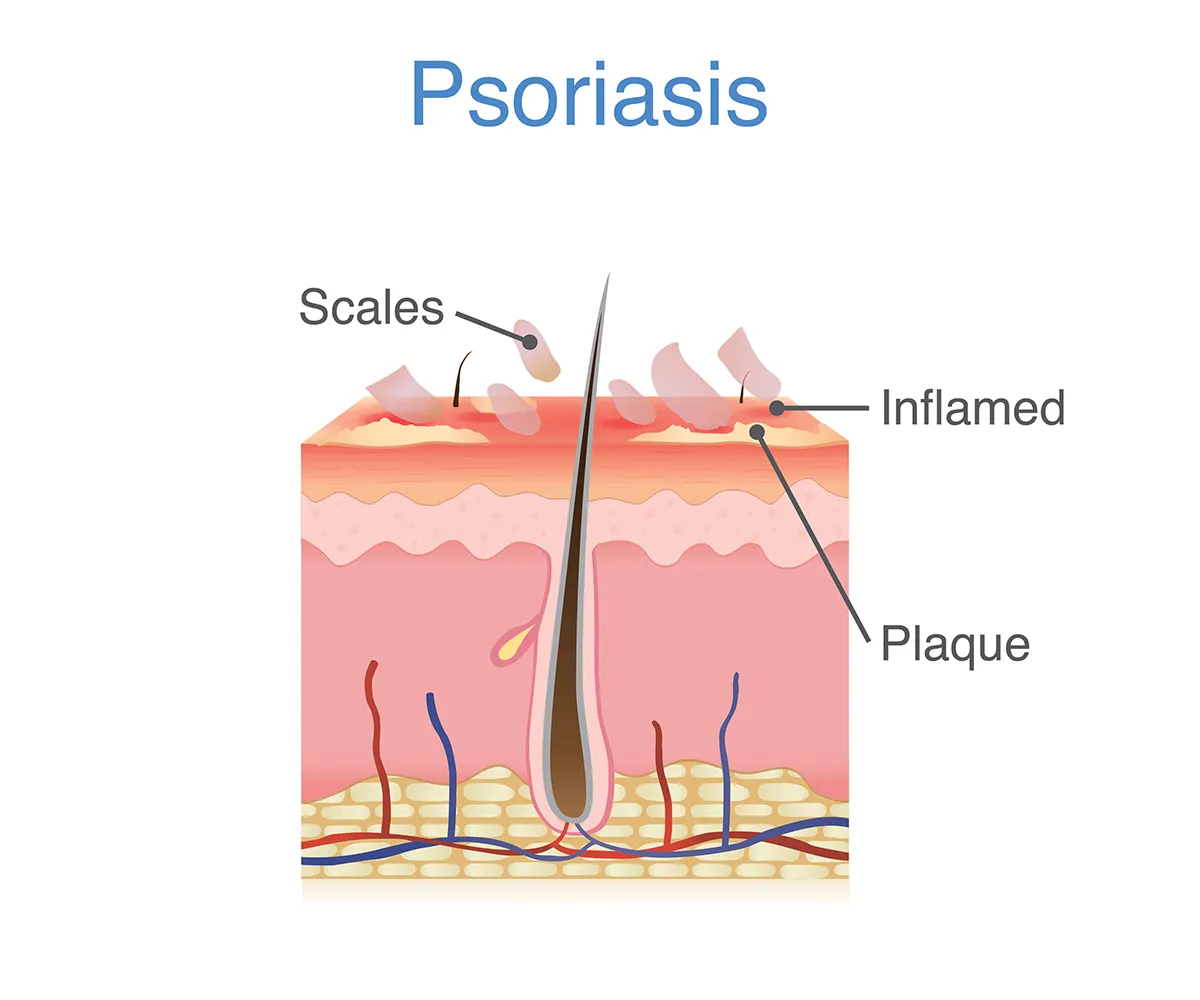
Symptoms of psoriasis often include inflamed, discolored skin with scaly patches called plaques.
Psoriasis is a common autoimmune disease that causes skin inflammation. If you have an overactive immune system, your body rapidly produces skin cells.
This increased skin cell turnover leads to a buildup of cells on the surface of your skin, resulting in the characteristic psoriasis rash.
Psoriasis can sometimes be mistaken for eczema, a common form of dermatitis that also causes rashes on your skin, or even skin cancer. It’s important to visit your doctor to rule out other conditions for your skin rash and get an accurate diagnosis.
Types of psoriasis
There are several types of psoriasis. The most common is plaque psoriasis. Some types only affect certain areas of your body, while others can appear anywhere. It’s also possible to have multiple types of psoriasis.
- Plaque psoriasis: Causes raised, red patches on your skin with white or silvery scales (plaques). The rash can be itchy and painful.
- Guttate psoriasis: Looks like red droplets or spots on your skin and is often caused by a bacterial infection like strep throat.
- Inverse psoriasis: A red, shiny and smooth rash that commonly appears in your skin folds, armpits, groin and skin folds.
- Erythrodermic psoriasis: A rare type that causes a red rash over most of your body that resembles a burn. It needs immediate medical attention as it can lead to chills, fever and dehydration.
- Pustular psoriasis: A rare type that causes raised white bumps filled with pus on your skin (pustules). You may feel sick and develop a fever, headache or muscle weakness and will need immediate medical attention.
- Palmoplantar psoriasis: A severe type of psoriasis where the skin on the palms of your hands and soles of your feet become raised, dry and thickened. In some cases, you’ll also develop pustular psoriasis bumps as well. This type can be painful, especially while walking or using your hands.
Your psoriasis may also be considered mild, moderate or severe:
- Mild psoriasis: Rash covers less than 3% of your body and includes isolated patches on your scalp and limbs.
- Moderate psoriasis: Rash covers 3-10% of your body and affects your arms, legs, scalp and torso.
- Severe psoriasis: Rash covers over 10% of your body and affects sensitive areas like your skin folds, face, bottoms of your feet and the palm of your hand.
Psoriasis symptoms
Symptoms of psoriasis are different for everyone. A psoriasis rash is cyclic, meaning it flares-up and then subsides. Common symptoms of psoriasis include:
- Patchy, discolored rash
- Dandruff-like silvery or white scaling
- Cracked, dry skin that may bleed
- Itching, burning or soreness
It’s common for a psoriasis rash to appear on your arms, legs and torso. Other common areas of your skin that psoriasis may affect include:
- Scalp psoriasis: Red, dry patches on your scalp that may include itching, bleeding, soreness, scaling and dandruff-like flaking.
- Facial psoriasis: Discoloration, dryness and scaling may appear in or around your ears, mouth and around your eyebrows and eyes.
- Genital psoriasis: A smooth, dry and discolored patch of skin may appear on or around your genitals.
It’s less common for psoriasis to appear on your hands and palms, feet and soles and your skin folds.
How does psoriasis make you feel?
Living with psoriasis can be challenging both physically and mentally. Depending on the type and severity of your condition, you may have discomfort that impacts your daily life. It’s important to work with your doctor to find a treatment plan that helps you manage your psoriasis.
What causes psoriasis?
Anyone can develop psoriasis, but you’re more likely to develop the condition if it runs in your family.
Certain lifestyle factors may increase your risk of developing psoriasis, including smoking, heavy alcohol consumption and obesity.
An illness that triggers the immune system can also cause psoriasis. This includes an ear infection, bronchitis or a respiratory infection.
Psoriasis triggers
You may notice your psoriasis rash comes and goes in cycles. Certain triggers may cause your psoriasis to flare-up or worsen, including cold weather, medications or even bug bites. Learning what triggers your psoriasis is important to managing the condition.
Common psoriasis triggers include:
- Stress
- Infections
- Cuts, scrapes, insect bites or sunburn
- Cold, dry weather
- Smoking
- Heavy alcohol use
- Lithium, beta-blockers and antimalarial medications
- Changes in hormones
Psoriasis complications
Sometimes psoriasis can lead to a condition called psoriatic arthritis. This condition causes pain, stiffness and swelling in the fingers, nails and joints.
If you have psoriasis, you’re also potentially at risk of developing other conditions such as:
- Temporary skin color changes: After plaques heal, the affected skin may show discoloration, either lighter or darker than the surrounding skin.
- Eye conditions: Psoriasis can increase the risk of eye issues, such as conjunctivitis and uveitis.
- Obesity: Those with psoriasis are more likely to be overweight, which can exacerbate the condition.
- Type 2 diabetes: There is a higher risk of Type 2 diabetes if you have psoriasis.
- High blood pressure: Psoriasis is linked to an increased risk of hypertension.
- Cardiovascular disease: The inflammation associated with psoriasis can contribute to heart disease and stroke.
- Other autoimmune diseases: Those with psoriasis may also develop other autoimmune conditions, such as celiac disease and Crohn's disease.
Diagnosing psoriasis
To diagnose psoriasis, your doctor will start with a physical exam. You’ll talk about your medical history, including any family history of psoriasis and autoimmune diseases, and any symptoms you are experiencing.
Other tests may be needed to confirm your diagnosis, including a skin biopsy so your skin cells can be examined under a microscope.
Psoriasis treatment
Your doctor will work with you to determine a treatment plan based on your type and severity of psoriasis. Mild psoriasis usually responds very well to topical treatments, including creams and ointments. Psoriasis treatment for moderate to severe cases typically includes oral or injected psoriasis medications and light therapy (phototherapy).
Other treatments for psoriasis may include:
- Steroids, usually prescribed as a topical steroid cream, such as cortisone cream
- Vitamin D creams
- Salicylic acid creams
- Topical or oral retinoids
- Anthralin creams, which can help treat stubborn, thick patches of psoriasis
- Methotrexate, an anti-cancer drug that interferes with the growth of skin cells
- Immunosuppressive medications
- Biologic medications (such as Enbrel)
- Medicated shampoos for psoriasis on scalp treatment
- Light therapy
How do you stop psoriasis from spreading?
It's important to follow your doctor’s care plan so you can manage your psoriasis during a flare-up. You should also avoid any triggers that make your psoriasis worse. If your rash is itchy, don’t scratch it – this could make your symptoms worse and lead to an infection.
During your psoriasis episodes, stick to a gentle skin care routine that uses mild, dermatologist approved products. You may also find that a diet high in anti-inflammatory foods such as leafy greens, nuts and seeds, and avocados can help.
Find a dermatologist
Find a dermatology specialist near you.
Get care
We help you live well. And we’re here for you in person and online.