Diabetic neuropathy
Find a neuro specialistDiabetic neuropathy is a complication of diabetes due to unmanaged blood glucose levels over a long period of time. High blood sugar damages the peripheral nerves throughout the body. However, diabetic neuropathy is more likely to damage the nerves in your feet and legs.
Depending on what nerves are affected, symptoms may include pain, tingling, numbness and weakness in the legs, feet and hands. It can also impact your heart, blood flow, kidneys and digestive system.
You may have mild symptoms, but diabetic neuropathy can be disabling and extremely painful for others.
If you have diabetic neuropathy, Aurora Health Care’s expert neurologists and endocrinologists will work together to help you manage your diabetic neuropathy symptoms and get your blood sugar under control to improve your quality of life.
What is diabetic neuropathy?
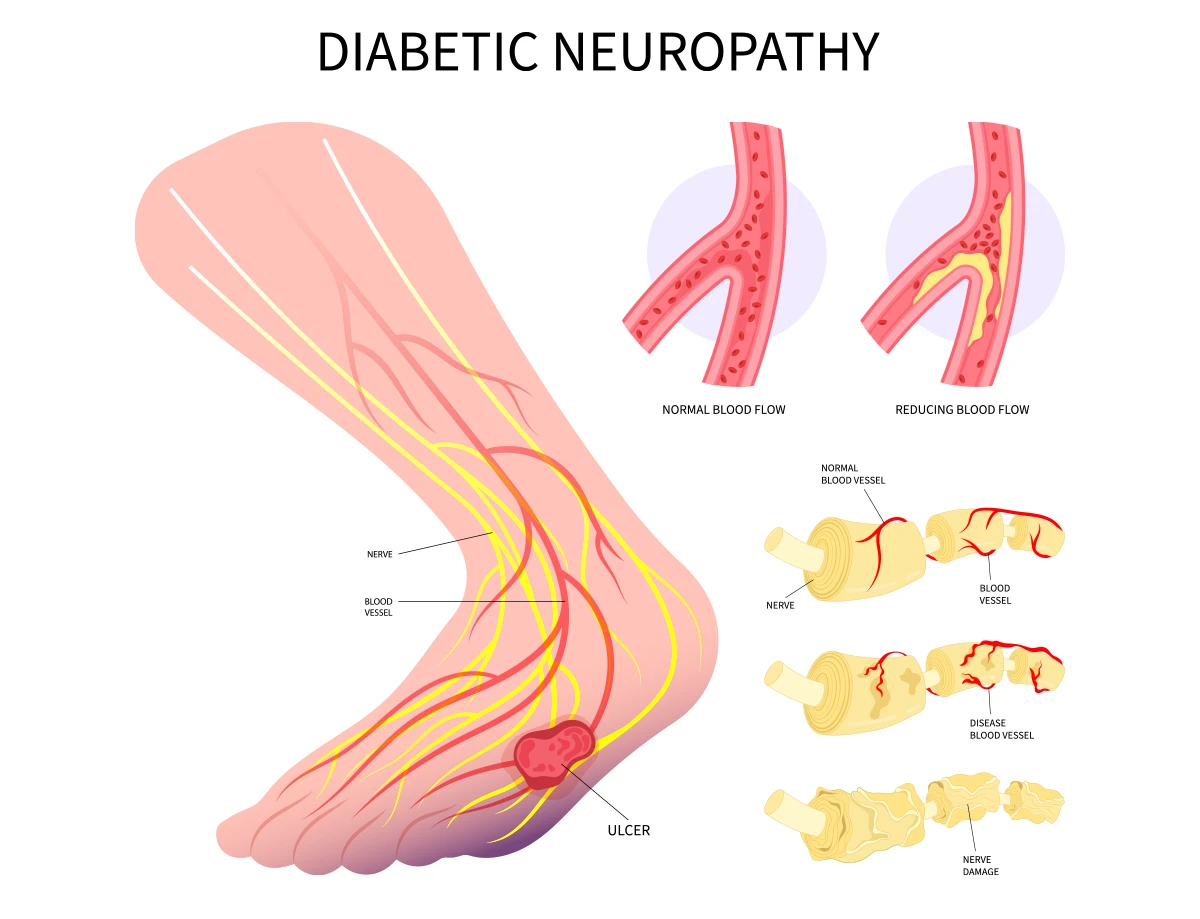
Diabetes damages your nerves and impacts their ability to carry messages to different parts of your body. The damage to these nerves, known as neuropathy, is caused by having high levels of glucose (sugar) in your bloodstream for too long.
Your doctor may refer to this nerve damage based on what nerves are impacted from high blood sugar levels.
The four types of diabetic neuropathy are:
- Peripheral neuropathy: Damage to the peripheral nerves in the hands, arms, legs and feet.
- Autonomic neuropathy: Damage to the autonomic nerves that control involuntary actions such as breathing, regulating body temperature and blood pressure.
- Proximal neuropathy: Damage to the nerves in the thighs, hips, buttock and legs. This is more common if you have type 2 diabetes.
- Mononeuropathy: Damage to a single nerve, usually to nerves close to the skin or near a bone.
If your neuropathy symptoms are felt in your feet or legs, your doctor may refer to it as diabetic neuropathy.
Risk factors for diabetic neuropathy
If you have diabetes, you are at a higher risk of developing neuropathy. More than 50% of people with diabetes will develop neuropathy. You’re more likely to have nerve damage from diabetes if you have any of the following risk factors:
- Family history of diabetes
- Kidney disease
- Being overweight
- Poor blood sugar control
- Smoking or excessive alcohol use
If you have any of the above risk factors or have been diagnosed with diabetes, regular checkups with your doctor can help reduce your risk of getting diabetic neuropathy.
Symptoms of diabetic neuropathy
Diabetic neuropathy symptoms vary depending on the specific nerve affected and the underlying cause of the condition. In most cases, diabetic neuropathy symptoms mirror those of other types of neuropathies, but are commonly felt in your feet and legs.
Some common symptoms of diabetic neuropathy include:
- Numbness or tingling: If you have diabetic neuropathy, you may experience numbness or tingling in your hands, feet and legs.
- Pain: Pain is a hallmark symptom of diabetic neuropathy.
- Sensory changes: For example, diabetic neuropathy can lead to changes such as loss of feeling or sensation in fingers, feet and legs.
- Sensitivity to touch: You may experience increased sensitivity to touch in the affected area.
- Temperature sensitivity: You may experience changes in sensitivity to temperature in your feet and legs, such as feeling excessively cold or hot.
- Weakness: Weakness in the muscles controlled by the damaged nerve is a common symptom. This weakness may impact your ability to stand on your feet or walk.
Symptoms of diabetic neuropathy develop gradually and may progress over time if the underlying cause is not addressed.
Diagnosis of diabetic neuropathy
Your doctor will ask about your diabetic neuropathy symptoms and anything that triggers or relieves them. They may also ask you about any alcohol or tobacco use, history of infections, diabetes and family history of neurological diseases.
Blood tests may be ordered to detect diabetes; vitamin deficiencies; dysfunction of the liver, thyroid or kidneys; infections or signs of abnormal immune system activity.
Your provider may also recommend nerve function and imaging tests such as a CT scan or MRI to identify any nerve damage.
Nerve function tests are also a valuable tool in diagnosing diabetic neuropathy. These tests include:
- Nerve conduction velocity (NCV) test: This test measures signal strength and speed along specific large motor and sensory nerves and reveals the location of nerve damage.
- Electromyography (EMG) test: For this test, tiny needles connected to electrodes are inserted into specific muscles to record their electrical activity at rest and during contraction. Test results show any abnormal muscular electrical and can help differentiate between muscle and nerve disorders.
Diabetic neuropathy treatments
There is no cure for diabetic neuropathy. Your provider will recommend treatment to slow progression, relieve pain, control blood sugar and manage complications.
The first step of treatment for diabetic neuropathy is to slow progression by managing blood glucose levels. Keeping your blood sugar under control may improve symptoms.
The next step will be to provide relief from the pain caused by diabetic neuropathy, usually through prescription medications.
Diabetic neuropathy medications include anti-seizure drugs or antidepressants. In some cases, antidepressants and anti-seizure medications are combined or used with over-the-counter pain medications such as acetaminophen or ibuprofen.
In some cases, your doctor may recommend buying orthopedic shoes to improve walking difficulties and help prevent foot injuries.
Physical therapy may also be recommended to learn muscle stretching and strengthening techniques that can help with pain relief.
Complications of diabetic neuropathy
If left untreated, diabetic neuropathy can cause serious complications that could lead to amputation of a toe, foot or leg.
Other complications of diabetic neuropathy include:
- Being unaware of low blood sugar levels
- Recurring urinary tract infections (UTIs)
- Incontinence
- Sudden drops in blood pressure
- Digestive problems
- Sexual dysfunction
- Increased or decreased sweating
You can prevent complications of diabetic neuropathy by managing your blood sugar levels and taking care of your feet.
Living with diabetic neuropathy
Living with diabetic neuropathy involves adapting to the challenges posed by nerve damage to maintain a good quality of life. The specific approach may vary depending on the affected nerve and the underlying cause of diabetic neuropathy.
Consult with your Aurora Health Care provider to receive a comprehensive treatment plan. Regular check-ups and open communication with your care team are vital to improve your quality of life with diabetic neuropathy.
Get care
We help you live well. And we’re here for you in person and online.