Invasive ductal carcinoma (IDC)
Find a cancer specialistInvasive ductal carcinoma (IDC) is the most common type of breast cancer, consisting of about 80% of all breast cancer cases. IDC is an invasive cancer that starts in the milk ducts and spreads into nearby tissue.
Our breast cancer specialists provide the best care in Wisconsin. We offer the most up-to-date cancer care technology, including genetic counseling to better determine your risk and a range of diagnostic tools to accurately diagnose cancer.
What is invasive ductal carcinoma?
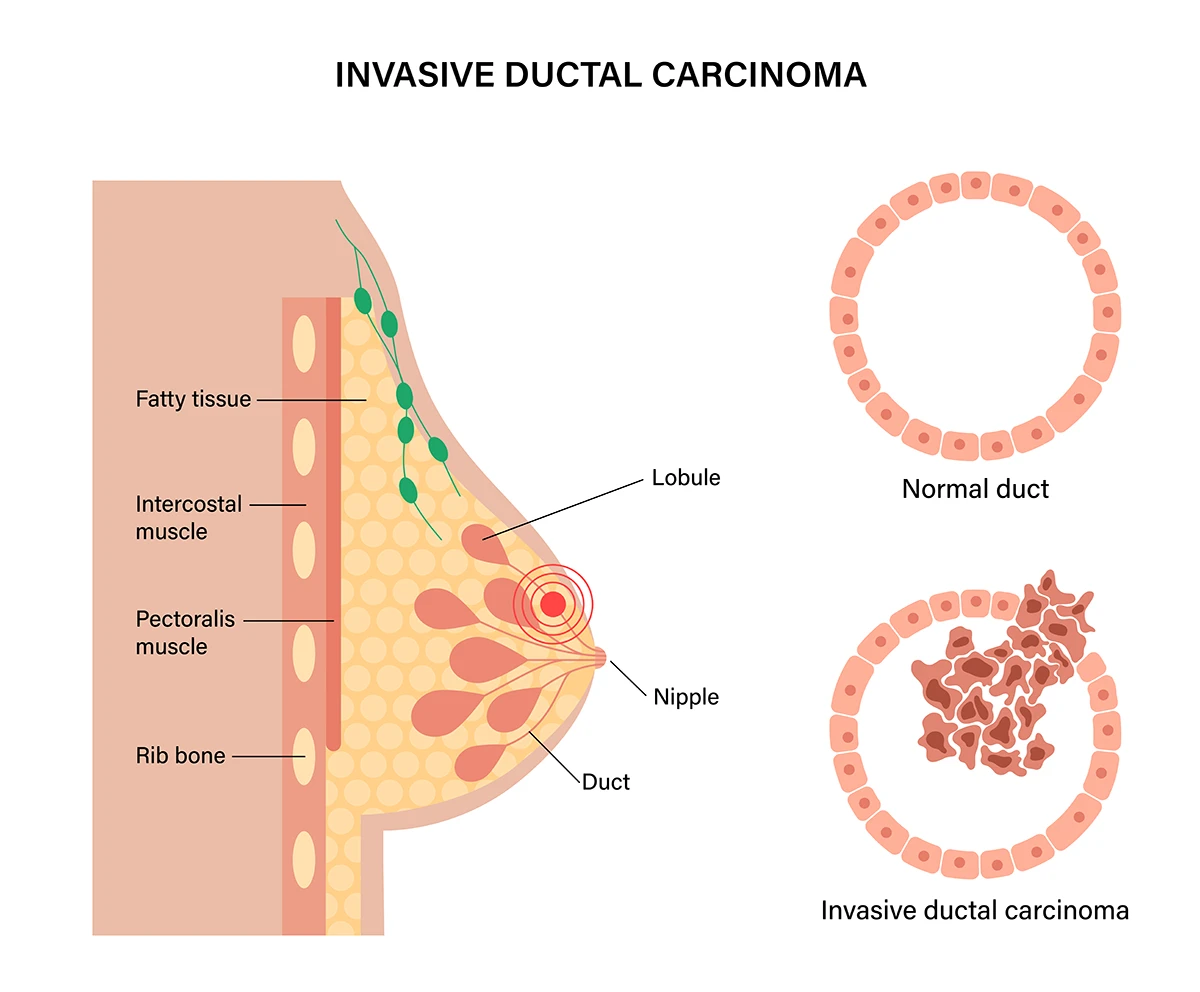
Invasive ductal carcinoma is breast cancer that has spread outside the milk duct of the breast.
Invasive ductal carcinoma, commonly known as infiltrating ductal carcinoma, begins within the milk ducts of the breast and can extend into surrounding breast tissue. Although predominantly found in women, men can also be affected by IDC and other types of breast cancer. Invasive ductal carcinoma is one of the more common breast cancers found in men.
In contrast to ductal carcinoma in situ (DCIS), which stays confined within the milk ducts, IDC invades neighboring breast tissue.
Invasive ductal carcinoma risk factors
Multiple factors contribute to the risk of developing invasive ductal carcinoma, ranging from family history, genetic mutations and lifestyle factors. If you have a family history of breast cancer, genetic testing can help assess your risk, especially for gene mutations associated with increased risk of breast cancer.
Other risk factors include:
- Age: While IDC can occur at any age, women over 50 are more likely to develop it.
- Dense breast tissue: Women with dense breast tissue on mammograms face an increased risk of both IDC and invasive breast cancer.
- Hormonal factors: Factors that affect hormone levels, like early menstruation, late menopause, childbirth after 30 and prolonged use of hormone replacement therapy may escalate IDC risk.
- Lifestyle factors: Obesity, excessive alcohol consumption and a lack of exercise can also contribute to a higher IDC risk.
- Personal history of breast cancer: A prior diagnosis of breast cancer in one breast increases your risk of developing IDC in the opposite breast.
- Radiation exposure: Past radiation therapy to the chest, especially during childhood or teenage years, increases the likelihood of IDC later in life.
Invasive ductal carcinoma symptoms
With invasive ductal carcinoma, you may not have any symptoms. This is especially true in the early stages of IDC.
The most noticeable signs of IDC include:
- A breast lump
- Changes in the appearance of your breast or nipple
- Breast discomfort or pain
- Swelling of your lymph nodes
It's common to discover these signs of IDC during a mammogram or breast self-examination.
If you detect any persistent changes to your breast health or encounter any of the symptoms, schedule an appointment with your doctor for an exam. To note, these symptoms may also be a sign of conditions unrelated to breast cancer, such as fibrocystic changes, infections or benign tumors.
Diagnosing invasive ductal carcinoma
To confirm a diagnosis of invasive ductal carcinoma, your doctor will start with a physical exam. They’ll discuss your symptoms and health history and perform a breast exam.
If IDC is suspected, imaging tests such as a mammogram, ultrasound or MRI may be used to help identify the grade of the tumor and investigate any suspicious areas. A biopsy may also be performed to better analyze suspicious tissue samples.
Following a biopsy or the removal of a lump, the tissue may undergo testing for:
- Hormone receptors: Hormone receptors are proteins on cell surfaces that bind to hormones like estrogen and progesterone. In certain cases, these hormones can stimulate the growth of cancer cells. If your cancer cells have too many hormone receptors for estrogen or progesterone, hormone therapy may be used as a targeted treatment to block these hormones.
- HER-2 status (also known as ErbB2): HER-2 is a gene that regulates cell growth, division and repair. Approximately one in four breast cancers exhibit an overabundance of the HER-2 gene. These cancers tend to grow rapidly. Determining the HER-2 status aids in tailoring treatment approaches to target this specific genetic characteristic.
Staging and grading are pivotal parts of the diagnosing IDC. By determining the IDC grade and stage of your cancer, your doctor can better understand the severity and aggressiveness of your cancer and determine your treatment plan.
Stages of breast cancer
Following your diagnosis, your care team will assess whether the cancer has spread and the extent of its spread. This process, known as staging, is vital for understanding the severity of the cancer and creating the appropriate treatment strategy.
Breast cancer stages span from stage 0 (carcinoma in situ) to stage IV (metastatic cancer). Generally, lower stages indicate less spread, while higher stages signify more extensive spread. Cancers in higher stages typically have a lower survival rate.
What is an invasive ductal carcinoma grade?
Invasive ductal carcinoma grade is a system used to classify the characteristics of cancer cells under a microscope.
The invasive ductal carcinoma grade system is a valuable tool in predicting the pace at which cancerous cells may grow and spread to nearby tissue.
IDC grading is on a scale ranging from one to three. One indicates the least aggressive and three is the most aggressive form.
- Grade 1 (low grade): Cancer cells closely resemble normal breast tissue cells. The cells tend to spread slowly, which makes this type the least aggressive.
- Grade 2 (intermediate grade): Cancer cells have some abnormal characteristics but aren’t as different as normal cells. These cells may grow and spread at a moderate pace.
- Grade 3 (high grade): Cancer cells have significant differences from normal cells. They are much more aggressive, rapidly growing and spreading to nearby tissue.
Treatment for invasive ductal carcinoma
Treatment options for invasive ductal carcinoma depends on your health history and IDC grade. Treatment typically involves a collaborative approach, aiming to kill all cancer cells and preventing cancer from returning.
Common treatments for IDC include:
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop their growth and division. It may be given before or after surgery.
- Lumpectomy (breast-conserving surgery): This surgical approach involves removing the cancerous tumor along with some of the surrounding healthy breast tissue. The surgery is often followed by radiation therapy to reduce the risk of recurrence.
- Radiation therapy: Utilizing high-energy beams, radiation therapy targets and destroys cancer cells.
- Mastectomy: In certain instances, a mastectomy, involving the removal of the entire breast tissue, may be recommended. Depending on your cancer grade and your personal preferences, a mastectomy might be followed by breast reconstruction surgery.
- Hormone therapy: This treatment is primarily utilized for hormone receptor-positive breast cancers, which is found in most cases of IDC. Hormone therapy functions by obstructing estrogen's effects or reducing estrogen levels in the body.
- Targeted therapy: Targeted therapy drugs are designed to specifically target molecules or pathways implicated in cancer growth and progression.
At Aurora, your care team will adopt a collaborative approach to deliver the best treatment for you. We also offer a variety of supportive care services, including counseling, nutrition therapy, palliative care and physical therapy.
What is the prognosis for invasive ductal carcinoma?
The prognosis for invasive ductal carcinoma depends on a variety of factors, including the IDC grade, whether there are estrogen and progesterone receptors present and the stage of the cancer. Generally, early-stage invasive ductal carcinoma, particularly those with low-grade tumors, typically have a more favorable prognosis.
Which invasive breast cancer has the best prognosis?
Among the different invasive breast cancer types, hormone receptor-positive tumors typically have the most favorable prognosis. These tumors have a better chance of responding to hormone therapy and have a reduced risk of recurrence in comparison to other types.
Are you at risk for breast cancer?
Knowing your chance of developing breast cancer can help you plan a routine screening schedule. Our breast health quiz estimates your five-year and lifetime risk and gives you an idea of what to do next based on your results.
Get care
We help you live well. And we're here for you in person and online.