Tubular breast cancer
Find a cancer specialistTubular breast cancer is a type of invasive breast cancer, which means it can spread to other parts of the body. Despite being invasive, tubular breast cancer is less likely to spread compared to other forms of invasive breast cancer because the cells are usually lower grade and grow slowly.
If you’re diagnosed with tubular breast cancer, our breast cancer specialists provide the best care in Wisconsin. We offer the most up-to-date cancer care technology, including genetic counseling to better determine your risk and a range of diagnostic tools to accurately diagnose cancer.
What is tubular breast cancer?
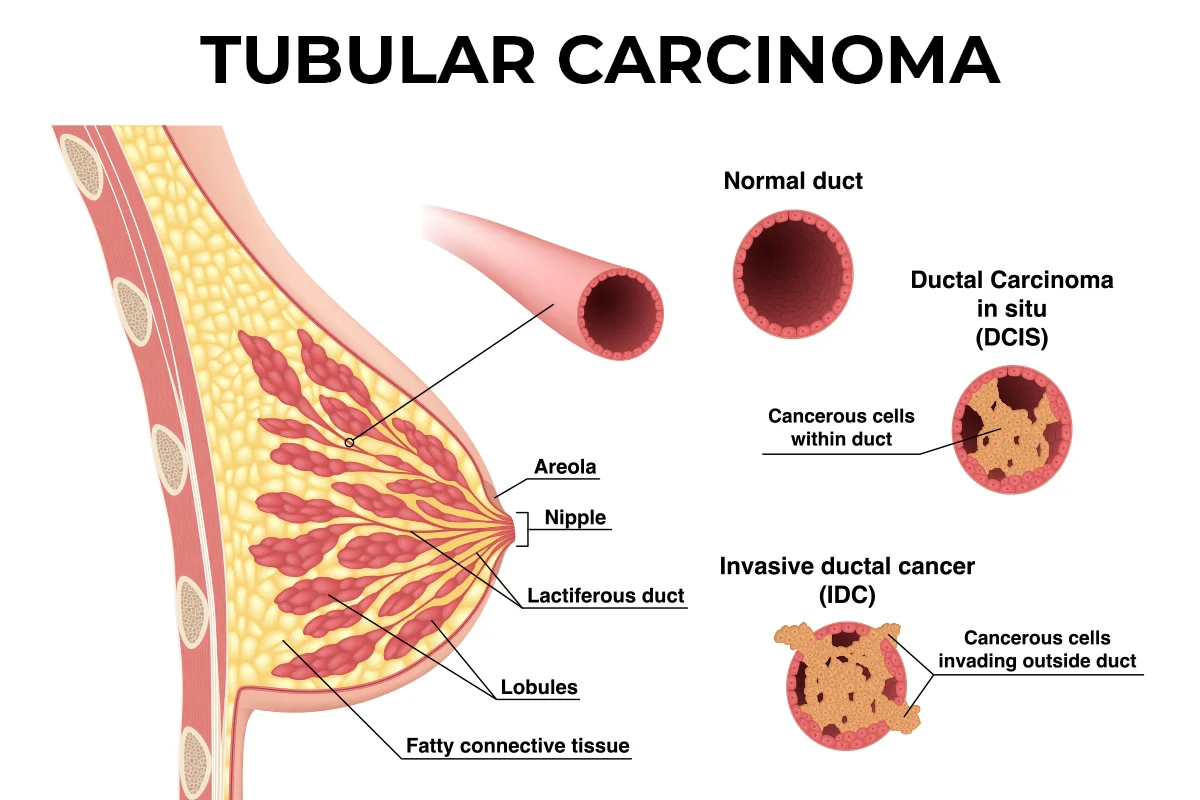
Tubular breast cancer is a rare type of invasive ductal carcinoma (IDC). It’s unique because of its tube-like characteristics and slow growth.
Tubular breast cancer, also known as tubular carcinoma, is a rare and specific type of invasive breast cancer.
Although it accounts for a small percentage of all breast cancer cases, the prognosis for tubular breast cancer is good. This type of breast cancer tends to have a lower risk of recurrence and a higher survival rate compared to other forms of invasive breast cancer.
What does tubular mean in cancer?
Tubular refers to the shape and arrangement of cancer cells. Tubular breast cancer cells form small tube-like structures, which is how the condition gets its name.
These tubular structures are generally well-differentiated, meaning the cells look more like normal, healthy breast cells. This can influence the behavior of the cancer and often suggests a better outcome compared to more aggressive types of breast cancer.
Risk factors of tubular breast cancer
While the exact cause of tubular breast cancer is not known, several risk factors can increase the likelihood of developing it, including:
- Age: Tubular breast cancer is more common in women over 50.
- Hormone replacement therapy: Long-term use of hormone replacement therapy (HRT) during menopause has been linked to an increased risk.
- Family history: A family history of breast cancer can elevate your risk, although tubular breast cancer itself is not typically considered hereditary.
- Early menstruation and late menopause: Women who start menstruating before age 12 or enter menopause after age 55 have a higher risk.
- Lifestyle factors: Alcohol consumption, lack of physical activity and obesity can also contribute to your risk.
Stages of breast cancer
Breast cancer is classified into stages based on the size of the tumor and the extent of its spread. The stages range from 0 to 4:
- Stage 0: Also known as ductal carcinoma in situ (DCIS), this stage is non-invasive and confined to the ducts of the breast.
- Stage 1: Early-stage invasive cancer where the tumor is up to two centimeters and has not spread outside the breast.
- Stage 2: The tumor is between two and five centimeters, or cancer has spread to a few nearby lymph nodes.
- Stage 3: Also known as locally advanced cancer, where the tumor is larger than five centimeters or has spread to several lymph nodes or nearby tissues.
- Stage 4: Metastatic cancer, where the cancer has spread to other parts of the body, such as the bones, liver or lungs.
Grades of tubular breast cancer
Cancer cells have characteristics that help identify its grade. Tubular cancer cells are most often low grade and are considered early stage.
When examined under a microscope, your care team can better understand your cancer and potentially predict the speed at which your cancer cells may grow and spread to nearby tissue or other parts of your body. Cancer cells will receive one of three grades:
- Grade 1 (low grade): Cancer cells closely resemble normal breast tissue cells. They exhibit slow growth and spread, meaning this grade is less aggressive.
- Grade 2 (intermediate grade): Cancer cells show some abnormal characteristics but are not visibly different from normal cells. They may grow and invade other areas of the body at a moderate pace.
- Grade 3 (high grade): Cancer cells appear significantly different from normal cells. They demonstrate aggressive behavior, including rapid growth and spread, often leading to a poorer prognosis.
Signs of tubular breast cancer
Tubular breast cancer often doesn't cause noticeable symptoms in its early stages. That’s why early detection through regular mammograms or monthly self-exams is crucial. Some signs to watch for include:
- A small, palpable lump: Usually firm and easy to move under the skin.
- Changes in breast shape or size: Any noticeable difference should be checked.
- Skin changes: Dimpling, puckering or redness on the breast skin.
- Nipple changes: Discharge, inversion or changes in the appearance of the nipple.
Diagnosing tubular breast cancer
Tubular carcinoma of the breast is diagnosed through a physical exam, imaging tests and a biopsy.
Your provider will check your symptoms, medical history and discuss any risk factors you may have. During the physical exam, they will feel for any lumps or masses in the breast.
Should your doctor suspect breast cancer, they’ll use various tests that may include:
- Imaging tests: Imaging studies such as ultrasound, MRI, CT scan or PET scan may be performed to visualize the tumor and assess its size, location and whether it has spread.
- Biopsy: A biopsy will be performed to obtain a tissue sample for examination under a microscope. This is the most definitive way to diagnose tubular breast cancer. Depending on the location of the tumor, the biopsy may be performed using a needle (needle biopsy) or by surgically removing a sample of tissue (incisional or excisional biopsy). A pathologist will examine the tissue sample to look for characteristic features of tubular carcinoma, such as tube-like structures.
Tubular breast cancer treatment
A combination of surgery, radiation and sometimes hormone therapy is commonly used to treat tubular breast cancer. The approach depends on the stage and specific characteristics of your cancer:
- Surgery: This is usually the first line of treatment and may involve a lumpectomy (removal of the tumor and some surrounding tissue) or a mastectomy (removal of the entire breast). The choice depends on the size and location of the tumor.
- Radiation therapy: Often follows surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Hormone therapy: If the cancer is hormone receptor-positive, meaning estrogen and progesterone can attach to the cells and help them grow, medications like tamoxifen or aromatase inhibitors may be used to block the hormones to stop the cancer's ability to grow.
- Chemotherapy: This is less commonly used for tubular breast cancer but may be recommended in certain cases, particularly if the cancer has spread to lymph nodes or other areas.
Your care team will use a collaborative approach to provide the best treatment possible. Supportive care services such as counseling, nutrition therapy, palliative care and physical therapy may also be offered to help you manage the physical and emotional challenges of cancer treatment.
What is the recurrence rate of tubular breast cancer?
One of the more reassuring parts of tubular breast cancer is its relatively low recurrence rate. Studies have shown that tubular breast cancer has a better prognosis and lower chance of recurrence compared to other types of invasive breast cancer.
Recurrence rates vary depending on several factors, including the stage at diagnosis and the treatments received, but overall, the outlook is favorable. Regular follow-up care and monitoring are essential to ensure any recurrence is caught early.
Are you at risk for breast cancer?
Knowing your chance of developing breast cancer can help you plan a routine screening schedule. Our breast health quiz estimates your five-year and lifetime risk and gives you an idea of what to do next based on your results.
Get care
We help you live well. And we're here for you in person and online.