When your brain activity is disrupted, you may slip into an unconscious state known as a coma. When this occurs, you won't be responsive or have any awareness of the world around you. A person can be comatose for a few hours, days or longer.
There are many reasons this loss of consciousness may happen, including due to a brain injury, infection, diabetes complication or loss of oxygen. Coma symptoms, outcomes and treatment depend on the severity and cause.
In certain situations, doctors may recommend a medically induced coma to prevent damage or allow the brain to rest and heal.
Comas are a medical emergency and require immediate treatment to avoid dangerous complications.
If someone is unconscious and unresponsive, call 911 immediately.
What is a coma?
A coma is a state of prolonged unconsciousness. You may appear to be in a deep sleep, but you won’t wake or respond to any stimulation – including pain. It’s possible for your body to make involuntary motor responses (generalized responses) or display spontaneous breathing.
It’s common to wake gradually after a coma within a few days or weeks. The length and severity of a coma depends on the underlying cause.
Comas range in severity. Doctors use the Glasgow Coma Scale (GCS) to assess a coma. GCS is a 15-point screening that evaluates eye, verbal and motor responses to check a person’s level of consciousness. The lower the score, the more severe the coma.
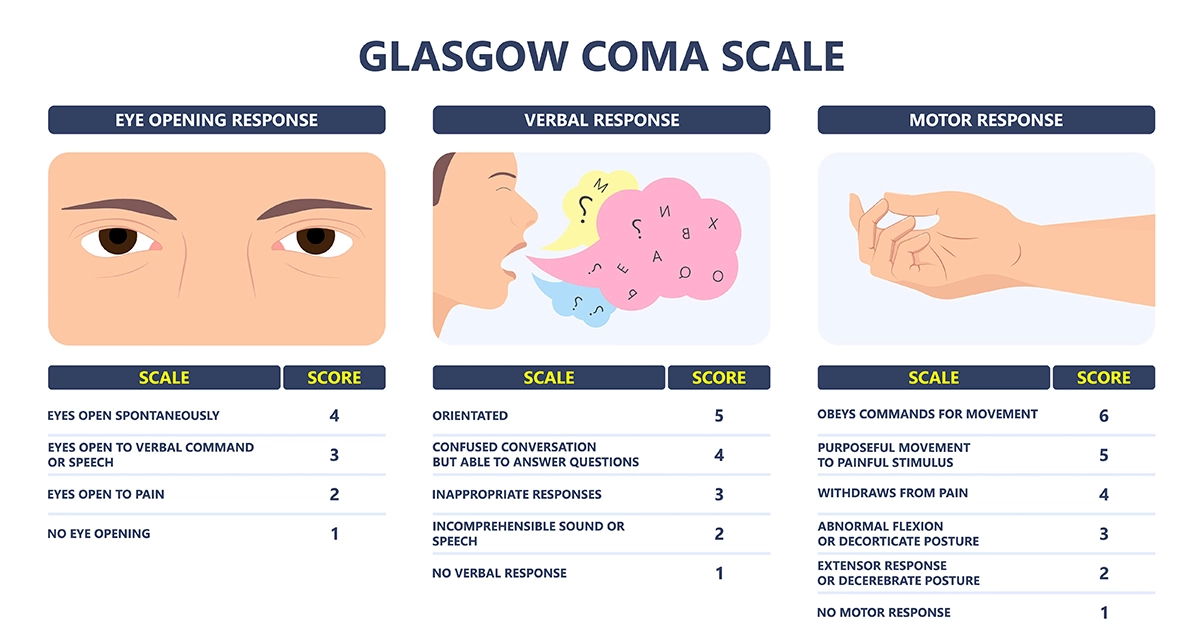
The Glasgow Coma Scale assesses a person’s level of consciousness and the severity of brain injury.
A coma requires around-the-clock medical care since you are unable to respond to your body’s needs. Sometimes important functions such as breathing and blood circulation are impacted during a coma. Medication and medical interventions, like a ventilator, offer support when this happens.
Comas due to a severe state of brain dysfunction may last longer – for months or even years.
Persistent vegetative state
Acute comas due to severe brain dysfunction are called a persistent vegetative state. If the coma is prolonged, breathing, nutrition and heart function assistance will be needed. This state can be permanent, but it’s possible to wake. Those that do wake usually don’t recover brain function.
Medically induced coma
After a serious medical emergency, a medically induced coma may be recommended to help prevent further brain damage. A controlled dose of anesthesia is used to temporarily induce a coma that is carefully monitored. This type of coma is usually used as a last resort.
Coma symptoms
There are three main symptoms that commonly define a coma. These include:
- Unconsciousness (a deep sleep with no response to stimuli)
- Lack of eye response (eyes closed with no response to light or movement)
- Lack of motor response (limbs don’t respond or voluntarily move)
Stages of a coma
There are four stages of a coma that follow a typical pattern. The length of each stage varies by person.
Your care team will closely monitor your vital signs and symptoms to track your stage and progress.
- Vegetative state: The active coma stage when you’re unresponsive to stimuli with closed eyes.
- Minimally conscious state: You’ll have slow or inconsistent responses to sound, touch or sight, including opening your eyes. This stage is one of the early signs of coming out of a coma.
- Confusional state: You’re responding more consistently but may be confused, agitated and have memory problems.
- Full consciousness: You can complete most routine tasks but need assistance. There may be personality changes that impact your judgement and decisions. During this stage, your doctor can assess any long-term complications of the coma and underlying cause.
What causes a coma?
There are many health conditions that may lead to a coma. A coma may also be the result of an acute event.
Common causes of a coma, include:
- Lack of oxygen to the brain (anoxic brain injury)
- Diabetes and blood sugar level extremes (diabetic coma)
- Brain tumors
- Extreme underactive thyroid (myxedema coma)
- Kidney failure
- Traumatic brain injuries (TBI), including concussions
- Toxins and poisons, such as carbon monoxide poisoning
- Metabolic imbalances (toxic-metabolic encephalopathy)
- Inflammation of the liver due to non-viral hepatitis
- Brain hemorrhage, such as an intraventricular hemorrhage (IVH)
- Stroke
- Infections, such as encephalitis, sepsis and meningitis
- Seizures
- Intracranial hypertension from conditions like hydrocephalus
Complications from a coma
During a coma, there are several complications that could develop, such as:
- Urinary tract infections (UTIs)
- Blood clots in the legs
- Pneumonia
- Bedsores
Other serious complications could result from the coma and underlying cause. This includes brain death. Brain death is the loss of all brain function after being placed on life support while in a comatose state. When this happens, there’s no chance of regaining consciousness. Brain death is usually the result of a severe and catastrophic brain injury.
Diagnosing a coma
It’s important to find the underlying cause of a coma to improve the outcome. Because there are so many factors, comas can be hard to diagnose.
Aurora Health Care’s team of expert neurologists will use the Glasgow Coma Scale to assess the severity of your injury. They’ll also perform a neurological examination and may order a series of tests that will help diagnose your condition and rule out other possible complications.
Common diagnostic tests include:
- CT scan: This is a noninvasive test that uses special X-ray equipment that captures many cross-sectional views of an organ or area being examined.
- MRI: This imaging test combines a powerful magnetic field, radio waves and a computer to create highly detailed images of the brain and other organs or body structures and their functions.
- Blood tests: A blood sample helps your provider measure abnormal levels that may indicate the source of the brain damage.
- Electroencephalogram (EEG): This test monitors brain wave activity.
- Lumbar puncture: Also known as a spinal tap, a lumbar puncture can diagnose diseases of the central nervous system, including the brain.
Coma treatment
Minimizing brain damage is the first priority of your coma treatment plan. Once the cause of the brain disruption is identified and you're stable, your care team will work with you to develop a personalized treatment plan that considers your condition, goals, and personal perspective.
Treatment options may include:
- Surgery
- Medications
- Neuroscience physical therapy
Recovering from a coma
Recovering from a coma can be a long process with several phases of recovery. Your age, type of brain damage and the severity of your coma all factor into how well you’ll recover.
Get care
We help you live well. And we’re here for you in person and online.