Intraventricular hemorrhage
Find a neuro specialistIntraventricular hemorrhage (IVH) is a serious medical condition that impacts brain function. It’s characterized by bleeding within the ventricles of the brain, which contain spinal fluid. When bleeding occurs, it could lead to long-term complications.
Getting prompt treatment is the best way to limit the impact of an intraventricular hemorrhage.
Call 911 or get to the nearest emergency department if you are experiencing symptoms of an intraventricular hemorrhage.
What is an intraventricular hemorrhage?
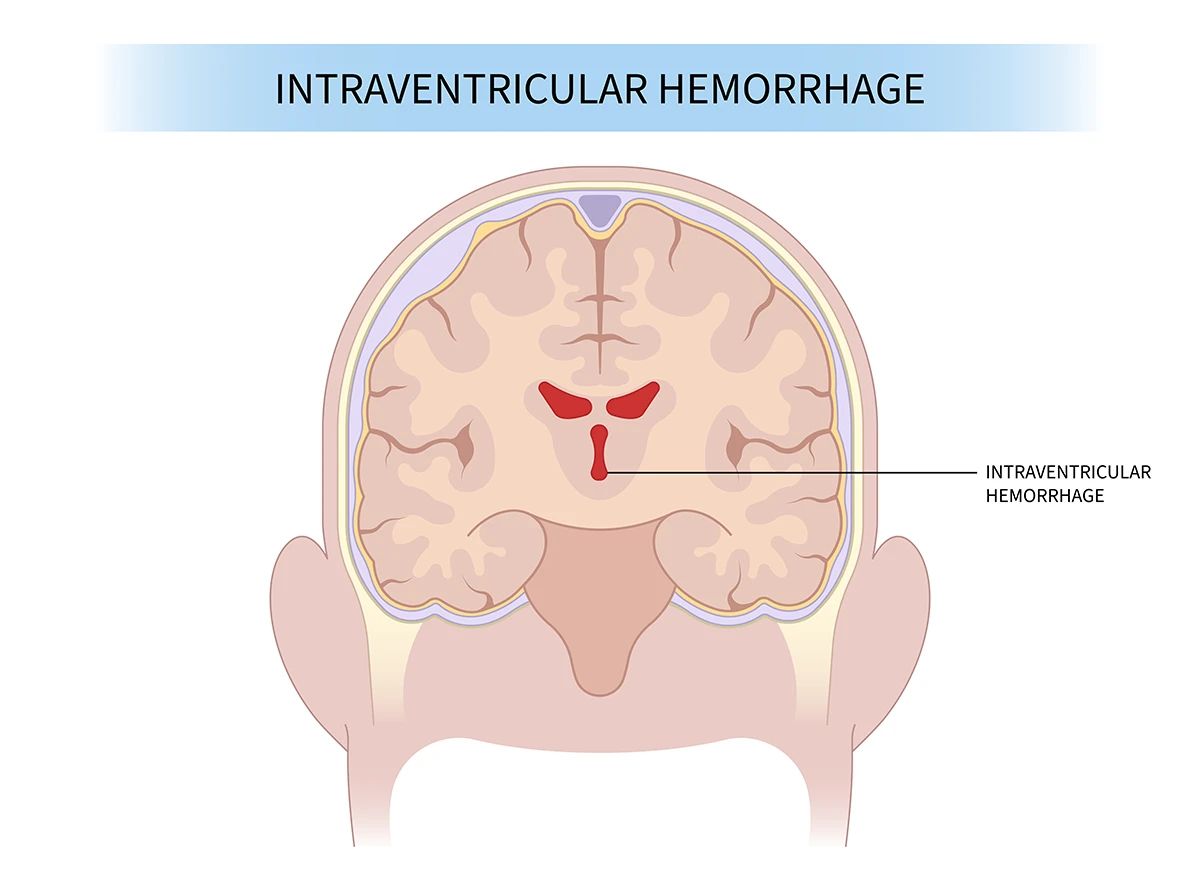
The location and size of an intraventricular hemorrhage in the brain.
An intraventricular hemorrhage is a type of brain hemorrhage where bleeding occurs within the brain's ventricular system, which is a network of fluid-filled spaces. The ventricles are responsible for producing and circulating cerebrospinal fluid (CSF), which protects the brain.
An intraventricular hemorrhage is more common in premature infants than adults, particularly infants born 32 weeks into a pregnancy. This type of bleeding happens when the tiny blood vessels in the germinal matrix (the fragile area of the developing brain) rupture and bleed into the ventricles. This area is more susceptible to bleeding due to developing blood vessels.
In some cases, an intraventricular hemorrhage may be fatal, while in others it may lead to long-term disabilities such as hydrocephalus (fluid buildup in the brain), developmental delays or paralysis.
Grades of intraventricular hemorrhage
Intraventricular hemorrhage is categorized into four different grades:
- Grade I: Bleeding is limited to a small amount in the germinal matrix.
- Grade II: Bleeding extends into the ventricles without causing significant dilation.
- Grade III: Ventricular dilation occurs due to the accumulation of blood.
- Grade IV: Severe bleeding with ventricular dilation, and it may also extend into the surrounding brain tissue.
Causes of intraventricular hemorrhage
There are many factors that can cause intraventricular hemorrhage. While most common in infants, an intraventricular hemorrhage can affect anyone. The most common causes include:
- Arteriovenous malformations (AVMs): These tangled connections between arteries and veins are prone to rupture.
- Aneurysm rupture: Aneurysms are weak bulges in blood vessel walls that can burst, causing internal bleeding.
- Blood thinners: Medications like aspirin or warfarin can increase bleeding risk, especially in combination with other factors.
- Brain tumors: Brain tumors can erode blood vessels or cause bleeding if they bleed themselves.
- Cerebral amyloid angiopathy (CAA): This condition involves protein buildup in brain vessels, making them fragile and prone to bleeding.
- Hypertension: Uncontrolled high blood pressure can weaken blood vessels, increasing the risk of rupture.
- Infections: Severe infections like meningitis can inflame and weaken blood vessels and lead to an intraventricular hemorrhage.
- Traumatic brain injury (TBI): Head trauma from accidents, falls or assaults can rupture blood vessels within the ventricles.
Symptoms of intraventricular hemorrhage
Symptoms of an intraventricular hemorrhage vary depending on the severity of the bleeding and whether it is affecting other areas of the brain.
Early symptoms that may be subtle include:
- Headaches
- Nausea and vomiting
- Vision changes
- Weakness
- Difficulty thinking or speaking
Common immediate symptoms include:
- Loss of consciousness
- Seizures
- Coma
Long-term symptoms:
- Hydrocephalus
- Developmental delays
- Learning disabilities
- Paralysis
Diagnosing and treating intraventricular hemorrhage
A prompt diagnosis is essential to providing effective treatment and minimizing complications of an intraventricular hemorrhage. To make a diagnosis, your doctor will review your medical history and perform a neurological exam to evaluate reflexes, balance and cognitive function.
Next, your doctor will use imaging testing such as a CT scan or an MRI to identify the severity and location of the bleed.
Intraventricular hemorrhage requires tailored individual treatment plans. There are different approaches for premature infants and adults.
Treating adults with an intraventricular hemorrhage
The first step is addressing the underlying condition that triggered the intraventricular hemorrhage, such as controlling high blood pressure, treating aneurysms, AVMs or stopping excessive bleeding due to medications.
Osmotic agents can be administered to draw fluid out of the brain and reduce intracranial pressure. Medications to control seizures and prevent blood clots may also be prescribed.
For severe cases with complications like hydrocephalus, surgical intervention may be necessary.
Treating infants with an intraventricular hemorrhage
The primary focus is on stabilizing the infant and protecting the developing brain. This includes maintaining vital functions such as breathing and circulation, preventing infections and controlling seizures.
Diuretics may be used to reduce the fluid’s pressure and prevent hydrocephalus. Certain medications can also promote blood clotting and minimize further bleeding.
In severe cases, minimally invasive surgery may be necessary to remove blood clots and relieve pressure within the ventricles.
Prognosis and outcomes of intraventricular hemorrhage
The prognosis for intraventricular hemorrhage is influenced by several factors, including severity, causation, timeliness of treatment, age and overall health.
Physical therapy, speech therapy and occupational therapy can help manage long-term effects and support individuals in regaining lost skills and functionality.
Complications of intraventricular hemorrhage
Intraventricular hemorrhage can lead to various long-term complications, especially if the bleeding is severe or if it occurs in premature infants. The extent of complications can vary based on factors such as the grade of hemorrhage, timeliness of treatment and the presence of associated conditions.
Some potential long-term complications include:
- Behavioral and emotional challenges
- Cerebral palsy
- Hydrocephalus
- Intellectual disabilities
- Learning disabilities
- Neurological Impairments
- Seizures
- Visual and hearing impairments
It's important to note that not everyone will develop these complications. Early detection, intervention and ongoing supportive care can play crucial roles in minimizing the impact of long-term complications.
Prevention of intraventricular hemorrhage
Preventing intraventricular hemorrhage involves addressing risk factors and implementing measures to reduce the likelihood of this condition, particularly in vulnerable populations such as premature infants.
Some strategies to prevent an intraventricular hemorrhage, include:
- Managing medical conditions like hypertension
- Avoiding head injuries
- Prenatal care for pregnant women at risk
- Make lifestyle changes and addressing maternal health issues
- Manage your blood pressure
- Wear protective head gear when riding a bicycle, motorcycle or at a job site
While these strategies can help reduce the risk of an intraventricular hemorrhage, it may not always be possible to prevent it entirely.
Are you at risk for stroke?
Most strokes are preventable, and many of the risk factors are controllable. Our stroke risk quiz will help you estimate your chances of experiencing one, find ways to minimize your risk and give you an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.