Occipital neuralgia
Find a neuro specialistHave you ever had a painful headache in the back of your head? It could be a rare headache disorder known as occipital neuralgia. This headache occurs when pain stems from the occipital region, or the back of your head, and spreads through the occipital nerves. The occipital nerves are at the top of your spinal cord and run up to your scalp. They control your head and neck.
Occipital neuralgia can be both a primary or secondary disorder, meaning it can either be its own condition or a symptom of an underlying disease.
There are several treatment options available to help you successfully manage the symptoms and pain from occipital neuralgia, especially if the underlying cause is treated.
While occipital neuralgia isn’t life-threatening, it’s painful.
What does occipital neuralgia feel like?
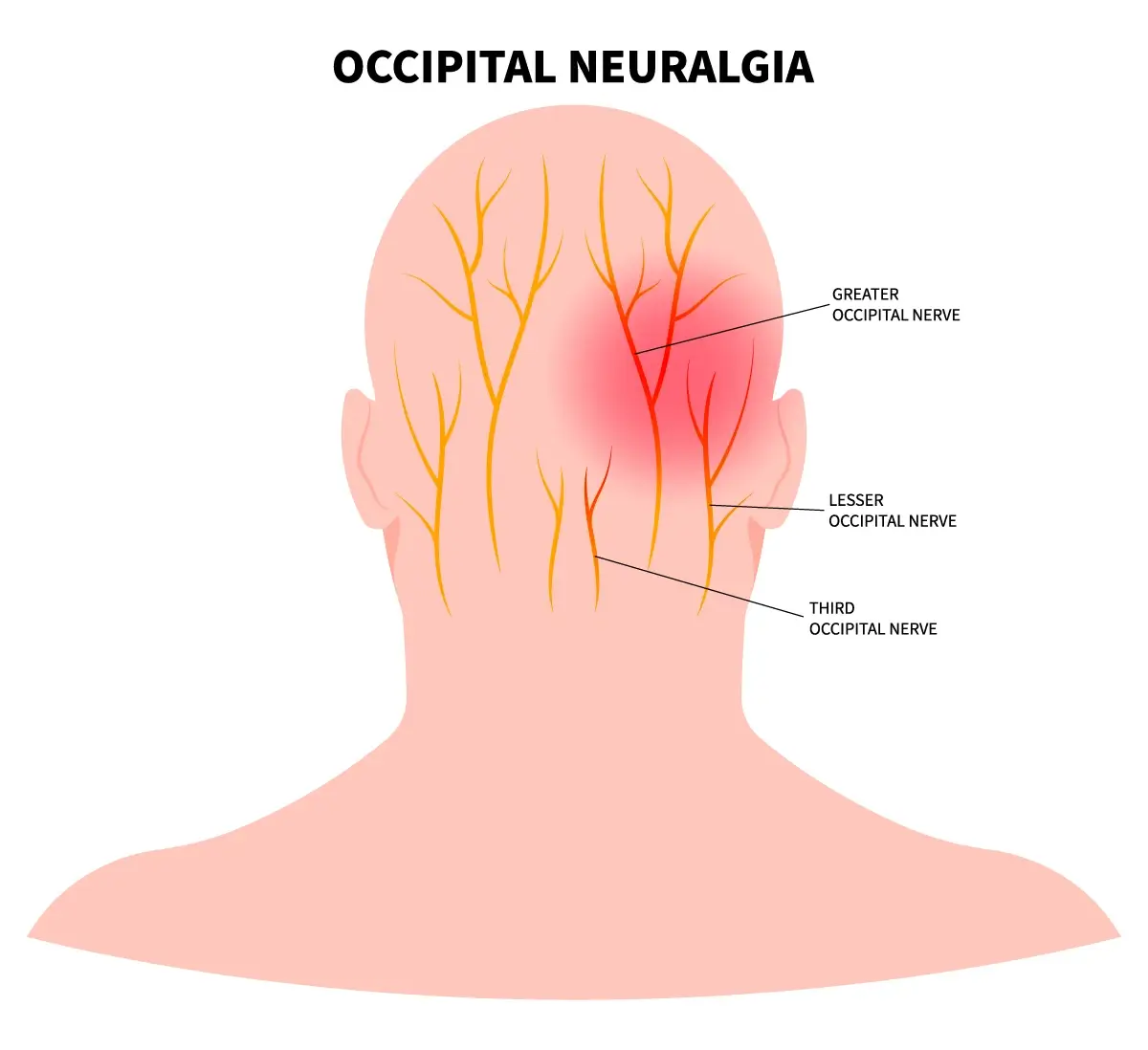
Pain from occipital neuralgia is felt in the back of the head in the occipital nerves.
Occipital neuralgia can feel like a sharp, shooting pain in the back of the head, usually on one side. It might be described as a throbbing or burning sensation. It can also cause sensitivity to light, scalp tenderness and pain behind the eye on the affected side. You may also feel pain at the base of your skull or behind your ear.
Unlike other headaches or migraines that slowly get more painful, occipital neuralgia can be triggered quickly, and by something as simple as brushing your hair. With occipital neuralgia, the severe pain is brief, lasting only a few seconds or a couple of minutes, and then goes away, whereas migraine pain is also severe, but lasts much longer.
Occipital neuralgia headaches are unlikely to have any symptoms such as drooping eye lids, eye redness or watery eyes. These symptoms are common with other primary headache disorders, such as migraines or hemicrania continua.
What causes occipital neuralgia?
Occipital neuralgia is commonly caused by pinched nerves in the root of your neck or because the muscles in your neck are too tight. In some cases, it can be caused by a head or neck injury.
However, since occipital neuralgia is also considered a secondary headache disorder, it can be a symptom of another condition. Conditions that may lead to or worsen occipital neuralgia include:
- Osteoarthritis, especially of the upper cervical spine, which can pinch nerves
- Tumors that grow on the nerve roots
- AVM (arteriovenous malformation)
- Brain aneurysm
- Brain tumor
- Meningitis
- Sleep disorders
- Stroke
- Sinusitis (inflammation of sinuses)
- Trigeminal neuralgia
- Rheumatoid arthritis
- Gout
- Infection
How is occipital neuralgia diagnosed?
Your provider will first do a comprehensive physical exam. They’ll ask about your medical history and how long you’ve been experiencing symptoms or if you have had any pain in the back of your head. One way your doctor may check to see if you experience pain is by applying pressure to the back of your head.
To check for an underlying cause, or rule out other conditions, your provider may order imaging tests such as an MRI or a CT scan. This will help them get a better look at your spine.
How do you get rid of occipital neuralgia pain?
In most cases, your doctor will recommend at-home treatments, such as applying a warm washcloth to the areas you feel pain and taking anti-inflammatory medications such as ibuprofen or naproxen. If you aren’t getting relief from those treatments, your doctor may prescribe muscle relaxers to relieve muscle tightness around the nerves.
If these more conservative methods don’t work, your doctor may inject a local anesthetic into your occipital area, or back of your head. This treatment can provide immediate relief and last for several hours.
For certain headache disorders like occipital neuralgia, an occipital nerve block can offer temporary relief. However, it's important to note that the effectiveness of nerve blocks can be different from person to person. Discuss nerve blocks with your doctor to determine if this treatment option is suitable for you.
In rare cases, your doctor may recommend surgery to reduce pressure on the impacted nerves, especially if the pressure is caused by an underlying condition such as rheumatoid arthritis or osteoarthritis.
Get care
We help you live well. And we’re here for you in person and online.